Male Infertility – Causes
What are the causes of infertility in men?
Infertility or subfertility in men has a variety of ways it manifests and a variety of possible causes. As we have described in the infertility section, infertility can mean:
- Decreased amount of semen volume
- Impaired functionality of spermatozoids
- Reduced production of spermatozoa
- Impaired sperm mobility (i.e. low motility)
- Difficulties in sperm transport
Each of the aforementioned manifestations of infertility / subfertility has its own individual causes.
Physiological Causes of Male Infertility
Α. Genitourinary infections
Genitourinary infections can primarily affect sperm functionality and volume. A series of inflammations can cause temporary or more serious and persistent problems to sperm. The most common of such infections are:
Chronic prostatitis (CP)
Chronic Prostatitis, which is found predominantly in young men with fertility problems, affects the sperm in many ways. Both the inflammation factor as well as the immune mechanism (caused by CP) create simultaneous outbreaks of infections in neighboring organs including the seminal vesicles, vas deferens, epididymis etc. Studies have revealed significant negative correlation of chronic prostatitis on sperm vitality, motility, concentration, functionality and liquification duration. When the male genitourinary tract is infected, bacteriotoxins, leukocytes, oxidative stress, and inflammatory factors (cytokines) may:
- Change the seminal plasma environment.
- Lead to the impairment of sperm motility.
- Induce sperm plasma membrane damage.
- Cause an autoimmune reaction.
- Contribute to the impairment of sperm cells.
- Lower sperm vitality.
- After ejaculation, semen forms a gel-like coagulum and within a 20-minute-period, the semen liquifies. The process is known as coagulation and liquification (i.e. “fibrinolysis”) and is mediated through the seminal vesicle protein system. Many enzymes, which are the essentials of semen liquification, and other liquification factors are secreted by the seminal vesicles and the prostate (e.g. PSA). Hence, prostatitis can change the duration of semen liquification as it affects those enzymes.
- A normal semen volume is necessary to carry the sperm into the female reproductive tract. Thus, semen volume is an important indicator of semen quality. Most of the semen volume is from the seminal vesicles, and approximately 1/3 of the volume is contributed by the prostate. However, these different fluids are not mixed until ejaculation. As such, prostatitis and the subsequent seminal vesiculitis may negatively affect the semen volume.
- A normal sperm concentration has at least 15 million spermatozoids per milliliter of semen. Moreover, sperm concentration is dependent on semen volume to some extent. Research shows that there is a negative association between chronic prostatitis with semen volume & sperm concentration.
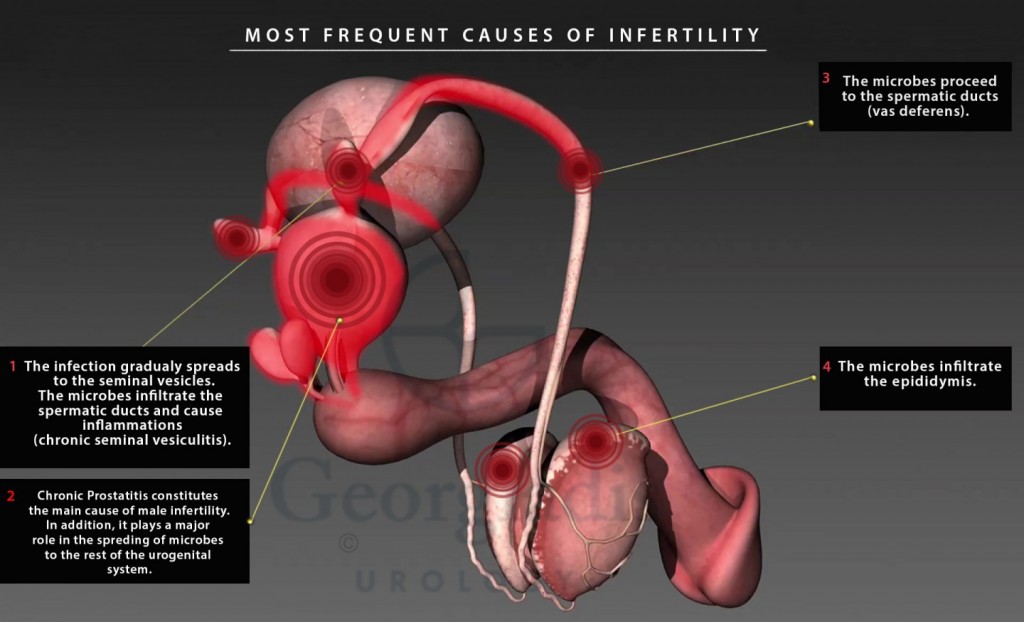
Figure 1: A visual representation of the most common causes of infertility due to inflammation. We can clearly see situations such as Chronic Prostatitis, Epididymitis, Seminal Vesiculitis and Orchitis. The aforementioned conditions can independently cause infertility, but it is worth mentioning that prostatitis can function as the original infector (leading to the other conditions). This is why we cannot stress enough how important it is to treat CP appropriately.
Orchitis
Inflammatory diseases that affect the testicles (after puberty) can create, in certain cases, infertility. Primary orchitis is typically observed along with the hematogenous spread of systemic, viral infections (e.g. mumps). Chronic granulomatous orchitis can occur with tuberculosis, syphilis or brucellosis. Epidemiological data gathered from infection-related orchitis have confirmed the increased risk of reduced ejaculate in the aforementioned orchitis cases.
Sexually transmitted diseases (STDs)
Chlamydia or gonococcal infections can also be associated with quality abnormalities in sperm. In men, infection by C. trachomatis can result in urethritis, prostatitis, epididymitis and orchitis. Studies regarding the effects of C. trachomatis infection on spermatogenesis, have shown disruption in the structure of the seminiferous tubules. In addition, they report loss of germ cells in a couple of weeks after the infection as well as severe injuries of the testicular tubules with only Sertoli cells. All the above have a progressively deteriorating effect on sperm count, motility and morphology of spermatozoa.
Seminal Vesiculitis
An infection to the seminal vesicles that stems from Chronic Prostatitis. It impairs the sperm functionality in the following ways:
- It decreases the volume of semen.
- Affects the coagulation-liquification mechanism.
- Affects motility by changing the spermatozoid propagation speed and way of movement.
Chronic epididymitis
From the perspective of etiopathogenesis, the notion that there is a connection between male infertility and epididymitis/epididymo-orchitis (resulting from STI-related urethritis and chronic prostatitis) seems plausible. The deterioration of sperm concentration observed in the ejaculate during the acute epididymitis is usually reversible within 3 months. However, there is a probability of 5% for azoospermia and 20% for oligospermia persisting despite patients claiming treatment of epididymitis. In practical terms, epididymitis is strongly correlated with infertility as:
- It causes obstruction in the channels (ductus epididymis, ductus deferens etc.)
- Damages spermatogenesis due to asymptomatic testicular inflammatory reactions
Interestingly, studies show that only 1/3 of infertility patients had unknowingly been through an episode of epididymo-orchitis in the past.
B. Varicocele
Varicocele refers to an abnormal enlargement of the pampiniform venous plexus. This causes valves’ failure that are supposed to prevent backflow. The mechanism by which varicocele affects sperm function is:
- Damage via excess heat caused by blockage to the blood pooling
- Oxidative stress on sperm
These effects alter the sperm environment causing problems with the quantity and mobility of the sperm.
C. Cryptorchidism
This is the failure of the testicle to descend from the abdomen into the scrotum. This causes the testicle to be exposed to higher temperatures than those in the scrotum, resulting in damage to spermatogenesis.
D. Hypogonadism
This is a condition where a hormonal disorder might stem directly from the testicle (i.e. primary hypogonadism) or a disorder/impairment in the center of the brain, from the hypothalamus or pituitary gland (i.e. secondary hypogonadism).
E. Chromosomal abnormalities
Inherited deteriorations of the testicles can affect sperm production. For instance, this happens with the Klinefelter Syndrome, an anomaly in which the male is born with two X chromosomes and one Y, instead of one X and one Y. This situation results in the abnormal development of the testicles.
F. Hormonal Abnormalities
Congenital deficiency of hypothalamic secretion of the substance GnRH (Kallmann Syndrome) can also affect fertility. This is because of the failure to release the necessary hormones for the sexual differentiation of organs and sperm production.
G. Sexual Issues
Problems with sexual intercourse or techniques may affect fertility. For instance:
- Difficulties with penile erection (i.e. erectile dysfunction)
- Premature ejaculation
- Pain during intercourse (i.e. dyspareunia)
- Various psychosexual problems
H. Congenital blockage of epididymis or vas deferens
Some people have congenital obstruction of the tube that:
- Stores the sperm when this moves out of the testicle (e.g. epididymis).
- Takes sperm from the testicle to the urethra (e.g. spermatic ducts).
I. Retrograde Ejaculation
This happens when the sperm appears to reflux towards the bladder, instead of the penis exit through the urethra. Diseases or factors causing such a condition are :
- Diabetes
- Incomplete closure of the bladder due to:
- Prostate surgery
- Urethral surgery
- Side-effect of certain medicines/drugs for known diseases
K. Absence of seminal fluid
Seminal fluid is essential for the transport of spermatozoa from the inner part of the genitals to the penis exit. It is meant to help spermatozoids ultimately reach the vagina. There are diseases that can cause an absence of seminal fluid, such as:
- Spinal cord injury
- Diseases of the nervous system
L. Hypospadias
Hypospadias refers to an abnormally-positioned urethral opening. There are three main types of hypospadias according to the position of the urethral opening:
- Penoscrotal hypospadias (i.e. the opening is near the scrotum)
- Midshaft hypospadias (i.e. the opening is in the middle of the penis)
- Subcoronal hypospadias (i.e. the opening is near the head of the penis)
The first two types create great difficulty in the sperm delivery to the vagina. In the case of subcoronal hypospadias there is no such problem.
M. Antisperm antibodies
These are antibodies produced against sperm antigens. Their presence is usually due to:
- A chronic inflammation of the urogenital system (e.g. prostatitis, epididymitis, orchitis etc.).
- A vasectomy (for men who have undergone this method of sterilization) resulting in weak or disorganized/disruptive sperm.
N. Cystic fibrosis
This is a disease which is usually combined with the absence or blockage of the vas deferens, which obviously blocks the transportation of the sperm.
Lifestyle & Environmental Causes of Male Infertility
There are cases where an individual’s health profile and the way they live create conditions which may affect potentially fertility.
I. Alcohol & Drugs
Increased consumption of alcohol and/or recreational drugs (e.g. amphetamines, opioids etc.) can affect fertility in the following ways:
- Lower sperm quality
- Reduced libido
- Impotence
- Deregulate hormone levels
II. Testosterone & Anabolic Steroids
An intake of hormonal substances for muscle gain (e.g. anabolic steroids) for a long period can also contribute to infertility. They can potentially:
- Shrink the testicles (as the natural hormone production is disrupted)
- Reduce sperm production
- Lower the quality & quantity of sperm
III. Smoking
Studies show that heavy smokers may suffer from moderate to severe abnormalities in their sperm as well as their erectile function.
IV. Emotional stress
Situations that cause intense feelings of anxiety, stress, etc., create conditions which disrupt spermatogenesis and can impact fertility. The main mechanism of this event is hormonal. In addition, the inability to fertilize may further lead to a worsening of the emotional situation, ultimately creating a vicious cycle.
V. Other medical conditions
Presence of tumor disease, kidney disease (e.g. kidney failure), liver disease (e.g. hepatitis or cirrhosis), major surgery, sickle-cell anemia etc., are all factors that contribute to a low sperm production.
VI. Age
Based on statistical data, age seems to affect fertility rate. However, there is no clear evidence whether this is attributed to age or a different pathogenic factor (e.g. prostatitis etc.).
VII. Poor Diet
Eating habits combined with a lack of certain nutrients or vitamins (e.g. vitamin C, selenium, zinc, folic acid etc.) can cause qualitative abnormalities in sperm.
VIII. Obesity
Hormonal and other abnormalities that develop in obese individuals, cause serious damage to sperm in several cases.
IX. Excessive heat to the testicles
Frequent and excessive use of saunas, or jobs in environments with high temperatures, cause problems with sperm production. Sedentary work, tight underwear or trousers which alter the temperature of the testicles can also cause infertility.
X. Insecticides & other chemicals
Τhe frequent use of insecticides and other chemicals on crops and agriculture can cause hormonal abnormalities. These can lead to an increase in estrogen, which has negative effects on sperm and increases the risk of developing testicular cancer. Exposure to lead also leads to infertility.
XI. Exposure to large doses of radiation
Continuous exposure to radiation leads to damage of the seminiferous epithelium, which can mean irreversible damage to a man’s fertility.
XII. Treatments for neoplasms
Both radiation and chemotherapy used to treat various cancers, negatively affect spermatogenesis. The closer the radiotherapy to the groin area, the greater the deterioration of the seminiferous epithelium.
