Impact of Chronic Prostatitis on Sexual & Erectile Dysfunction
How does Chronic Prostatitis cause Sexual / Erectile Dysfunction?
As we have explained in the introductory section of sexual disfunction, the central cause of erectile dysfunction is overwhelmingly the chronic inflammation in the prostate (CP). This is regardless of if CP is the only factor or if it exists in combination with other factors (e.g. lifestyle, psychology etc.).
Common Scenarios of Misdiagnosis
There are three common scenarios that make doctors misdiagnose the root cause of ED as something other than CP:
- They diagnose CP correctly, but they are unable to treat it. For example, a doctor recognises a prostate inflammation from lower urinary tract symptoms and the tests were positive for microbes. The antibiotics diminish the inflammatory edema temporarily and then there is full relapse. In other words, the pharmaceutical treatment for CP is unsuccessful. As such, they assume that prostatitis is not the causing factor of ED.
- They misdiagnose CP for pelvic pain syndrome because the microbiological exams show negative. For instance, a patient has felt inflammation with mild or minor symptoms (either irritative or obstructive) in addition to ED. The subsequent microbiological tests show negative results and the patient is therefore diagnosed with chronic pelvic syndrome (CPPS). The next step is a misguided treatment plan that of course has no effect on the erectile dysfunction symptom. Needless to say, it is also futile for the underlying Chronic Prostatitis that the patient is unaware of. Ultimately in this scenario, after their CPPS treatment fails, they typically attribute ED to psychological etiology.
- Symptoms of Chronic Prostatitis are confused with symptoms of other prostate diseases. Consider a case where the visible symptoms are of the obstructive nature. Such symptoms are: urination problems, low flow, feeling of incomplete emptying of the bladder etc. Doctors often attribute these to prostatic hyperplasia, and thus they suggest a wrong treatment plan which usually includes surgery. In fact, it is the Chronic Prostatitis that has caused both the hyperplasia as well as the erectile dysfunction.
How does CP cause Erectile Dysfunction?
Chronic prostatitis affects the penile tissue, which in turn causes the erectile dysfunction. There are two main mechanisms that cause ED:
- First Mechanism: Relating to inflammatory agents that are released during inflammation.
- Second Mechanism: Relating to neural damage that happens due to the expansion of the inflammation to the periprostatic genital nerves.
These mechanisms explain a number of physiopathological changes that take place on the dysfunctional penile tissue during chronic prostatitis.
First Mechanism – Inflammatory Agents
Endothelial Lesions
CP generates a systemic inflammatory response (i.e. spread through the blood) that impairs the endothelial function of corpus cavernosum. During the chronic inflammation process in the prostate the following chain reaction takes place:
- Cytokines and cellular adhesion molecules, which are both products of the inflammation, cause lesions in the endothelium.
- This in turn leads to endothelium inflammation within the vascular wall, which leads to dysfunction of the vascular wall. This means that the wall becomes less elastic and thus it has impaired ability to relax.
- The next stage is atherosclerotic lesions in the penile vasculature, which is what actually leads to erectile dysfunction. Effectively, the aforementioned phenomenon works as an impairment in the penile blood flow during the erectile process.
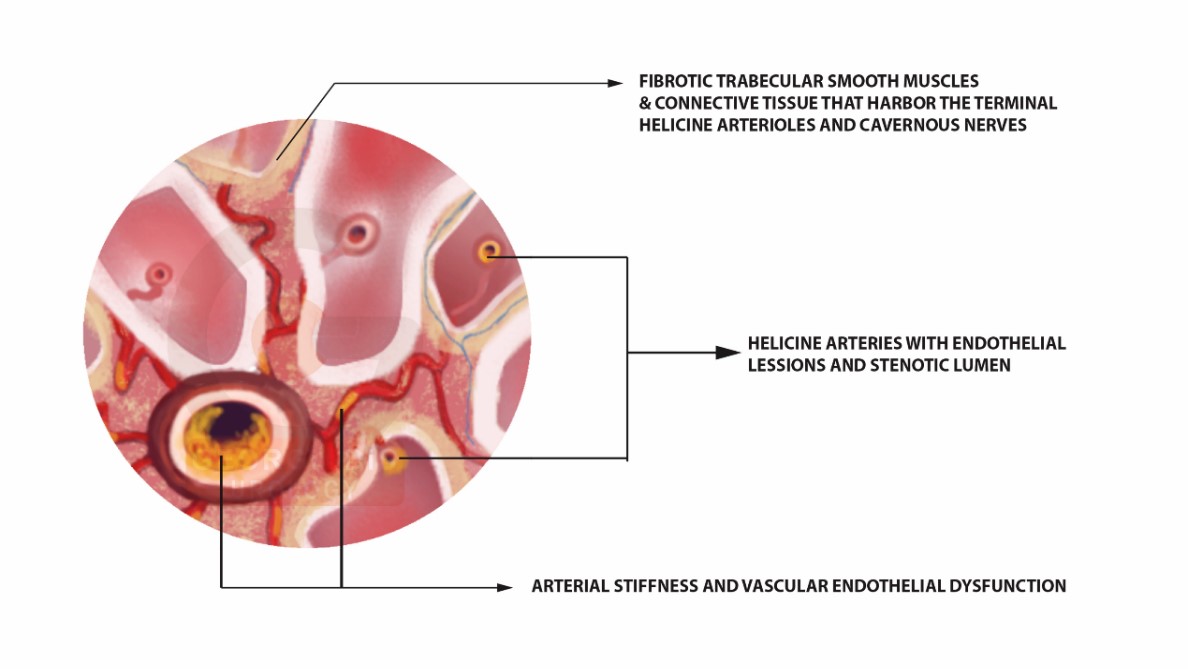
Figure 1: Visual represantion of the changes in the erectile / cavernous tissue. As we can see at the center of the image, there are lesions in the endothelian. These lesions reduce the vascular lumen and thus reduce the incoming (arterial) blood flow. In addition, we can see the fibrosis in the smooth muscle tissue resulting in the inability of the caversnosal spaces to expand. This inability causes the failure to stop the blood loss from the rigid erection. Effectively, the veno-occlusive mechanism is altered, resulting in semi-rigid erections.
Decreased eNOS & cGMP
Nitric Oxide (NO) synthesized and released from cavernous endothelial cells by endothelial nitric oxide synthase (eNOS) is an important factor in penile erection. Chronic inflammation in the prosate, produces cytokines and markers of inflammation that inhibit the expression of eNOS in endothelial cells and reduce its biological activity. As a result, the mechanism that relaxes the vascular wall and smooth muscular penile tissue underperforms which further results in ED.
The cyclic guanosine monophosphate (cGMP) is known as an important component in penile erection and is positively correlated with NO production. The cGMP and eNOS expression levels are all decreased significantly in CP patients. Studies show that CP/CPPS impairs the endothelial function via the eNOS/NO/cGMP signaling pathway.
We can thus conclude, that chronic prostatitis increases arterial stiffness and vascular endothelial dysfunction.
Oxidative Stress
The correlation between chronic prostatitis and oxidative stress are of utmost importance. Oxidative stress and inflammatory cytokines play a critical role in the pathologic process of CP/CPPS and the aggravation of symptoms. Much of neuronal and endothelial damage has been attributed to oxidative stress. Several previous studies have indicated an important role for reactive oxygen species (ROS) in the pathogenesis of ED, through the overproduction of superoxide, resulting in the acute impairment of penile relaxation and long‐term vasculopathy of corpus cavernosum.
Corporal apoptosis (i.e. corpus cavernosum death of cells) resulting from oxidative stress in penile tissues is a major cause of erectile impairment. To our knowledge, both oxidative stress and apoptosis cause smooth muscle cell and endothelial cell damage in corpus cavernosum tissues. The results of different studies show that patients of chronic prostatitis associated with ED had high levels of oxidative stress and apoptosis.
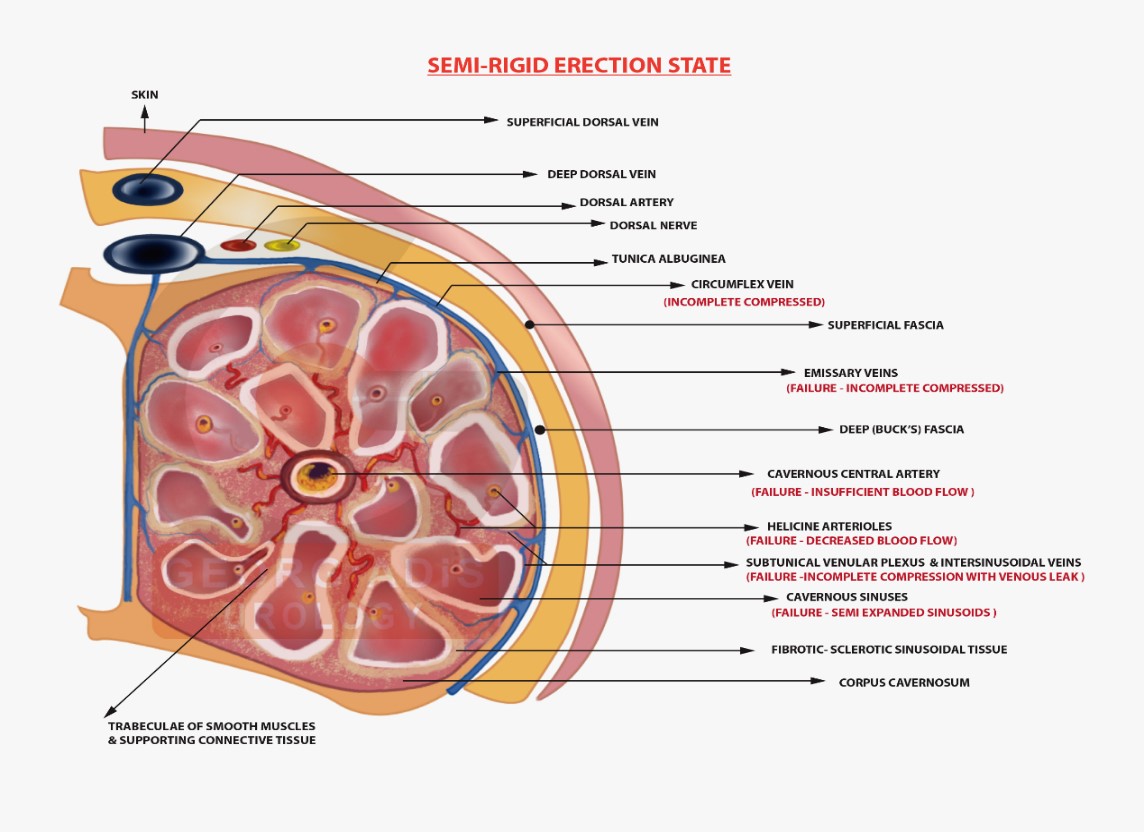
Figure 2: Visual representation of erectile dysfunction (semi-erect penile state). We can see the cavernosal tissue with diffuse fibrotic lesions. The incomplete compression of the emissary and intersinusoidal veins leads to venous leak due to the incompetence of the fibrotic sinusoidal spaces. Cavernosal (central) artery sclerosis with stenotic lumen due to endothelial lesions causes diminished (insufficient) blood flow. Helicine arterioles with strictures and sclerotic lesions with insufficient blood movement. Incomplete expanded fibrotic sinusoids with decreased elasticity and compliance, that fail to dilate fully and are unable to fill the corpus cavernosum with enough blood in order to cause a complete erection.
Corporal Fibrosis
Loss of corporal smooth muscle cells within the corpus cavernosum and the replacement of these cells with collagen characterizes ED. This results in the increase of corporal fibrosis. Increasing evidence demonstrated that CP/CPPS inflammation and the resulting oxidative stress may play important roles in pathological mechanisms of corporal fibrosis. Corporal fibrosis plays a key role in the deterioration of ED, by decreasing penile elasticity and compliance. The ratio of collagen to smooth muscle content determines the degree of corporal fibrosis – the higher the collagen the worse the fibrotic lesions. Due to this imbalance, the penile tissue loses its elasticity and again this contributes in ED.
Second Mechanism- Neural Damage
Genital Nerve Strangulation
The cavernous nerves from the peri-prostatic nerve plexus carry the sympathetic and parasympathetic nerve signals. These nerves are responsible for the vascular changes which cause erection and detumescence (i.e. reduction in volume). The inflammatory process spreads in all the prostate tissue from the central periurethral zones (i.e. prostate tissue around the urethra) towards the periphery and thus expands to postero-lateral areas. When the inflammation reaches those areas, it:
- Infiltrates the tissue which surrounds the genital nerves.
- Causes an edema that strangulates the nerves progressively.
- Alters the signal along their course.
- Ultimately, produces a down-regulation in permanent cavernosal tissue stimulation.
The reduced neural signals, in turn, cause a chronic decrease in blood flow, oxygen and antioxidative agents. This effect induces oxidative stress, muscle apoptosis and increases collagen production. Cavernous corporal fibrotic lesions are slowly established which in turn lead to a decreasing penile elasticity and compliance. It is worth mentioning, that this is in addition to all the other similar mechanisms mentioned before.
The result is an impairment of penile cavernosal tissue relaxation, along with vascular endothelial lesions which in turn lead to an increased arterial stiffness. The compromised elasticity of the cavernosal penile tissue further aggravates the blood flow, resulting in permanent and progressing erectile dysfunction.
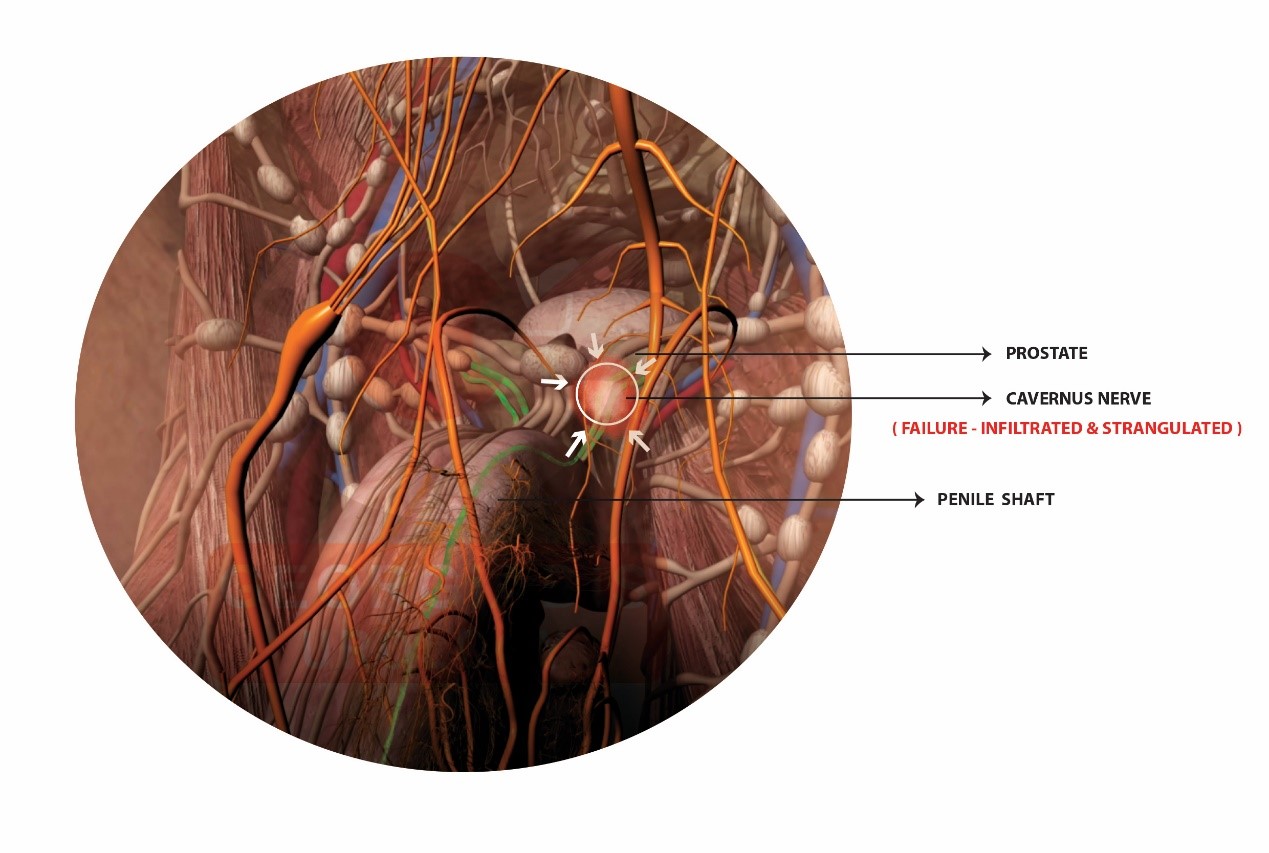
Figure 3: Visual representation of the cavernous nerve inflammatory infiltration. Inflammatory process from the prostate gland spreads into the pericavernosal nerve tissue, causes edema and nerve strangulation. That progressively impairs the cavernosal nerve function by altering the signal along their course, thus producing a down-regulation in cavernosal tissue stimulation.
Conclusion
To summarize, we have presented are a number of different mechanisms caused from Chronic Prostatitis that collaborate, often coexist and ultimately lead to erectile dysfunction.
As such, it should be clear by now that there can be no permanent cure of erectile dysfunction, unless we first properly treat Chronic Prostatitis.
For this purpose, we have developed our specialised:
- Georgiadis Chronic Prostatitis Protocol (GCPP) – for Chronic Prostatitis
- Georgiadis Erectile Revivification Protocol (GERP) – for Sexual & Erectile Dysfunction