Varicocele
What is Varicocele?
Varicocele means a moderate to high degree of venous plexus distention in the scrotum. In other words, it is an enlargement of the veins in the scrotum. These veins are components of the spermatic cord and their function is to drain blood from the testicles. Varicocele often resembles varicose veins that we see in people’s legs.
Varicocele is a common cause of reduced sperm production and poor sperm quality. That being said, in 30%-40% of varicocele cases, despite this anatomical problem, the sperm remains intact/unaltered.
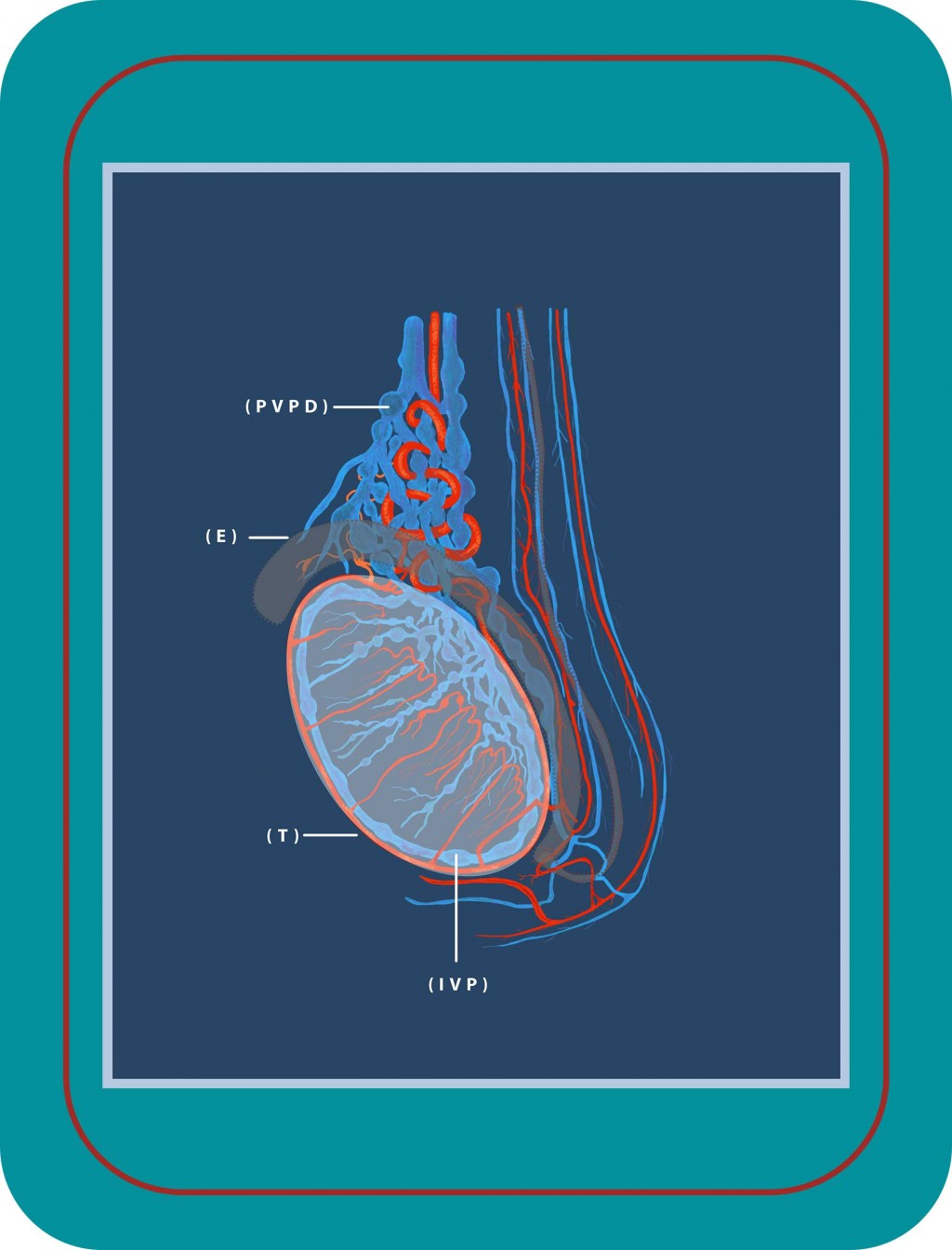
Figure 1: Graphical presentation of arteries and veins that supply the testicle (T) and epididymis (E). We see the varicocele pathology with dilated veins over the testicle (pampiniform plexus, PVPD) and inside the testicle (intratesticular venous plexus, IVP).
The development of varicocele is relatively slow and its diagnosis isn’t particularly difficult. Thus, if this condition causes problems to a patient, a doctor can successfully operate it immediately and at low risk.
Symptoms & Signs of Varicocele
Usually there is no particular discomfort with this condition. This may be a problem as it makes varicocele harder to detect for a patient.
In a few cases there is moderate pain. This pain is variable and can manifest as:
- Feeling of discomfort in the scrotum.
- Slight feeling of heaviness in the scrotum.
- Intense feeling of scrotal pain after:
- Sitting or standing for several hours
- Physical exercise or other heavy lifting activity.
Usually the pain disappears or simply becomes imperceptible when the person rests or lies down.
When should someone seek medical assistance?
As varicocele is not obvious, patients (or couples) only find out when they visit the doctor for infertility issues.
Patients should seek medical help, in cases where they:
- Feel heaviness or intense pain in the scrotum.
- Detect a lump/mass on the scrotum.
- Experience swelling in the testicle or scrotal area.
Causes of Varicocele
The function of the seminal veins is to drain blood from the testes. They achieve this by a mechanism which relies on the good condition of a venous valve system. The movement of these valves transfers blood in contrast to gravity. So, if this system is damaged, blood begins to reflux into the veins causing them to dilate/distend. This establishes the phenomenon of venous failure.
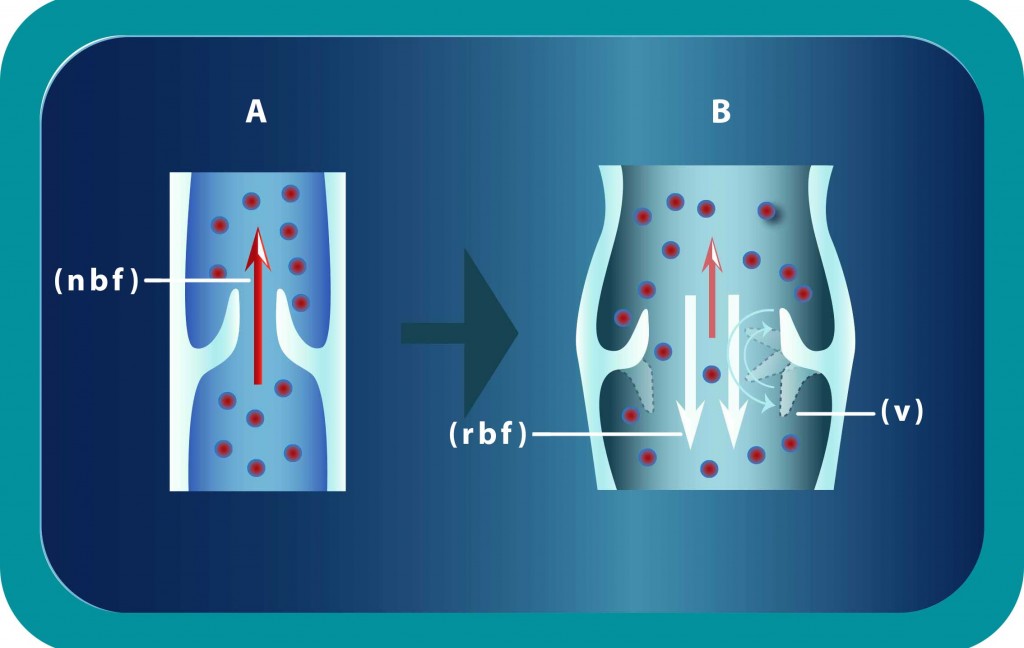
Figure 2: A. Graphical presentation of the normal venous blood flow (NBF) against gravity. B. Incompetent valves (VV) fail to push blood against gravity and we have reverse venous blood flow (RBF) inside the spermatic veins.
Intra-abdominal pressure
Intra-abdominal pressure during childhood and adolescence increases in many instances. We consider it as a common predisposing factor for varicocele development.
Anatomical factors
In addition, it appears that anatomical factors contribute to varicocele creation. More specifically, the left spermatic vein is:
- Straighter than the vein on the right side.
- Ending vertically to the renal vein.
- Longer than the opposite one.
These cause downward pressure inside the vein which ultimately leads to the condition of the varicocele.
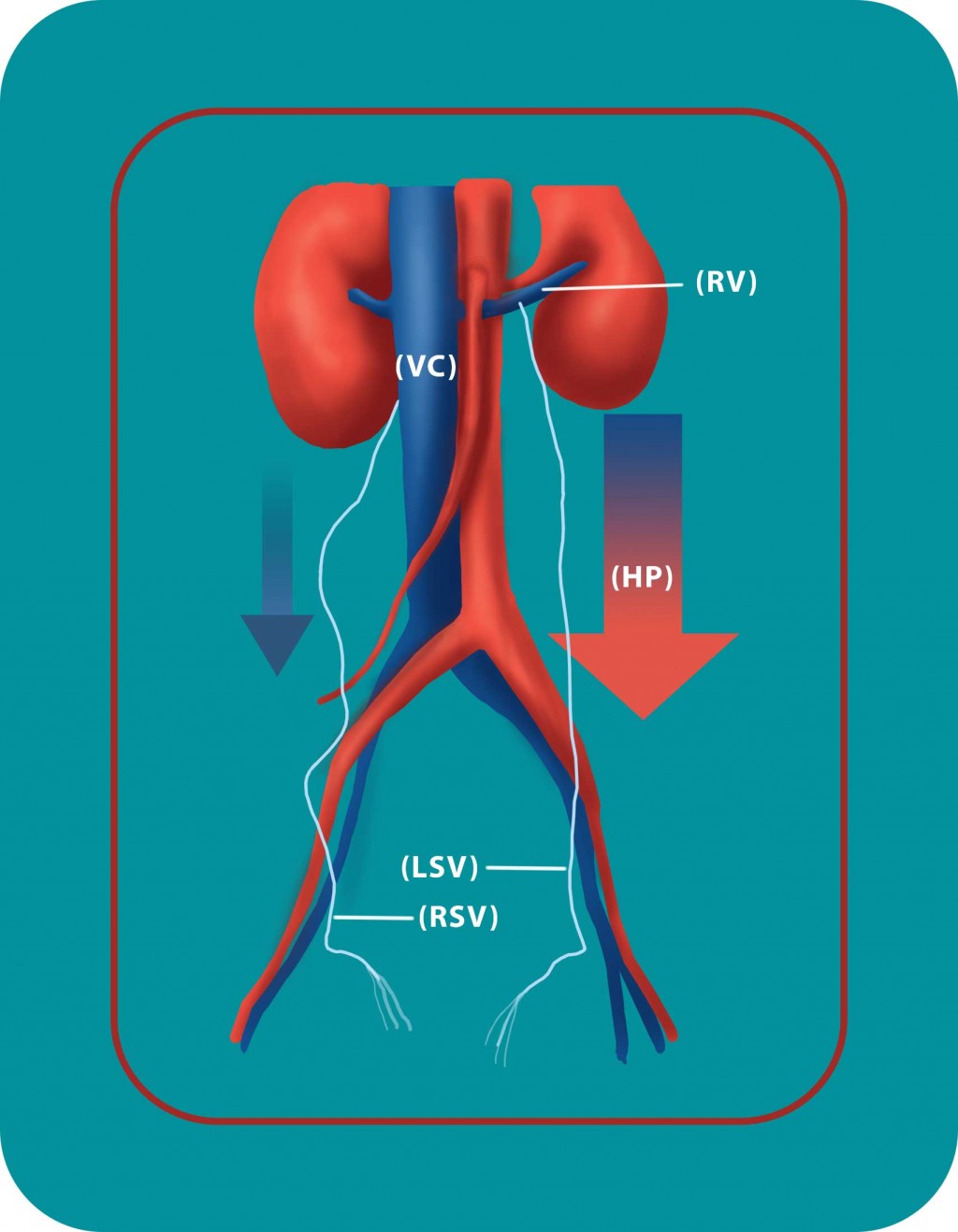
Figure 3. The left spermatic vein (LSV) is longer than the opposite one (RSV) and ends vertically to the renal vein (RV). A greater downward pressure (HP) is created inside the vein which leads to varicocele in this side.
The Nutcracker Syndrome
In some cases, there is an artery to the intestines that comes from the anterior part of the aorta. During its pulsations, it might squeeze the renal left sided vein which passes through the space between aorta and anterior mesenteric artery. This causes the blood to backup in the left testicular vein. As a result, this leads to a higher hydrostatic pressure and a reverse blood flow in the spermatic vein. This is what we call the “Nutcracker syndrome”.
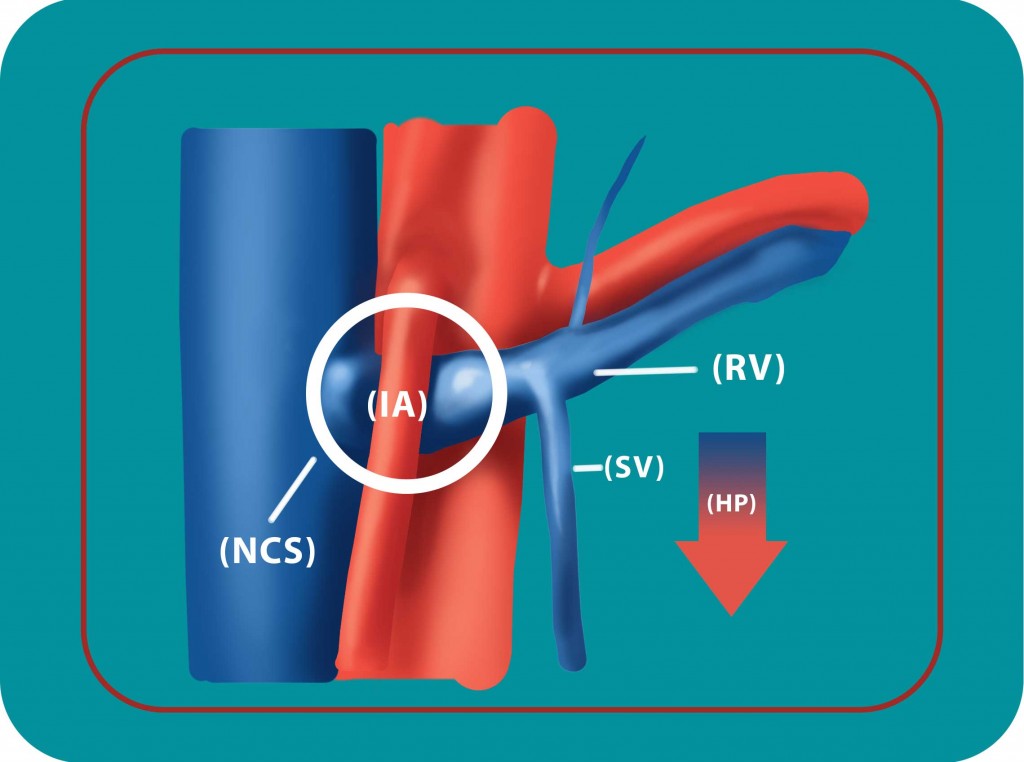
Figure 4: The Nutcracker Syndrome (NCS). The pulsations of the intestinal artery (IA) squeeze the left renal vein and cause the blood to back up in the left testicular vein (SV). This leads to high hydrostatic pressure (HP) and reverse blood flow in the spermatic vein.
Mechanisms & Pathology of Varicocele
Pathological changes that take place during varicocele are:
- Stasis and reflux inside the spermatic venous plexus.
- Under-oxygenation of testicular tissue for a long period of time.
- Elevation of scrotal and testicular temperature (hyperthermia).
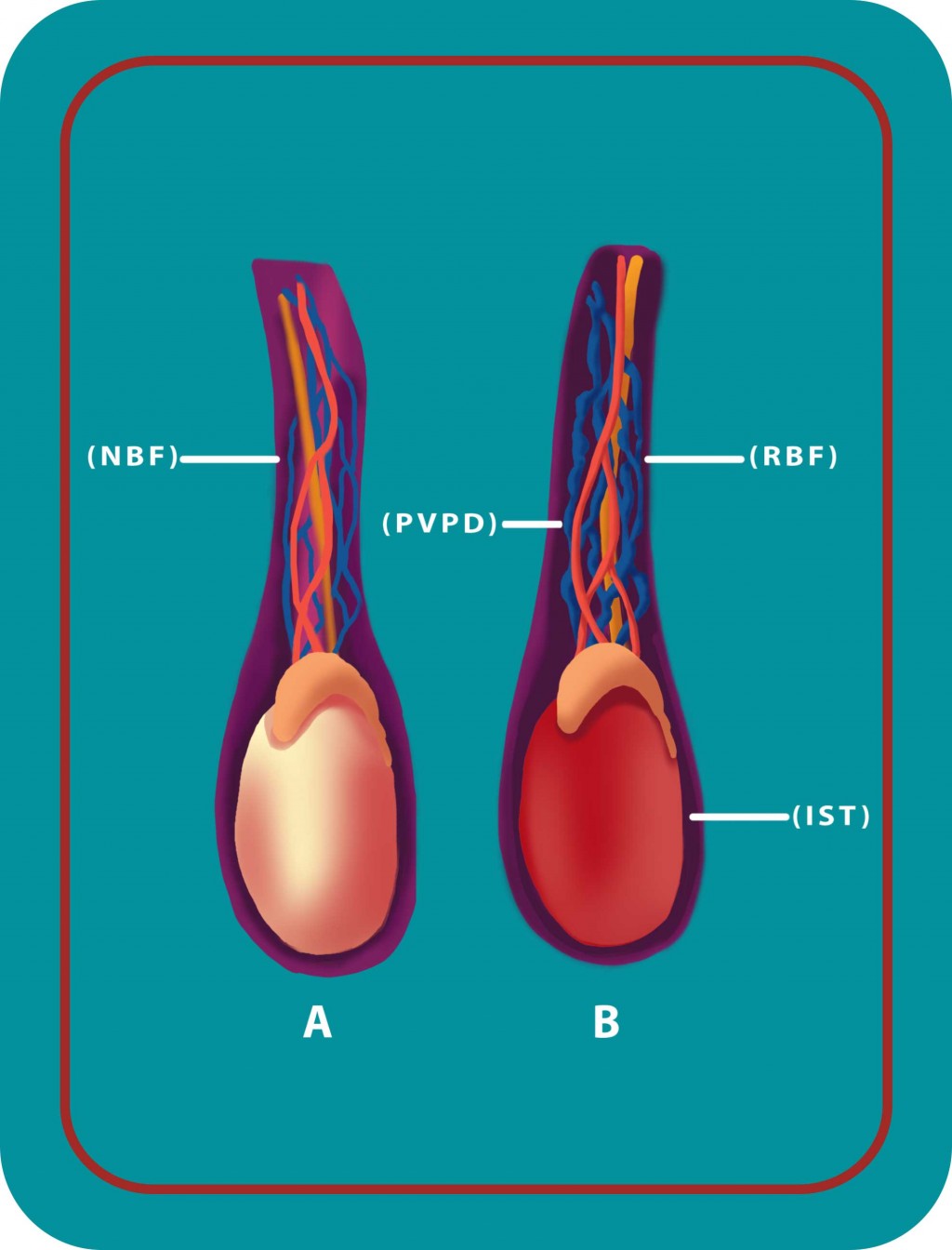 Figure 5: A. Normal blood flow (NBF) inside the spermatic veins, with normal scrotal temperature. B. Pampiniform venous plexus dilated (PVPD) with reverse blood flow (RBF) and increased scrotal temperature (IST).
Figure 5: A. Normal blood flow (NBF) inside the spermatic veins, with normal scrotal temperature. B. Pampiniform venous plexus dilated (PVPD) with reverse blood flow (RBF) and increased scrotal temperature (IST). - Progressive degeneration of the seminiferous epithelium.
- Negative effect on testicular endocrine function (reductions in testosterone synthesis by Leydig cells).
- Alteration of protein metabolism in the testicle’s tissue.
- Reduction in Sertoli cell function.
The aforementioned pathology is what leads to problems in the quantity and motility of the sperm.
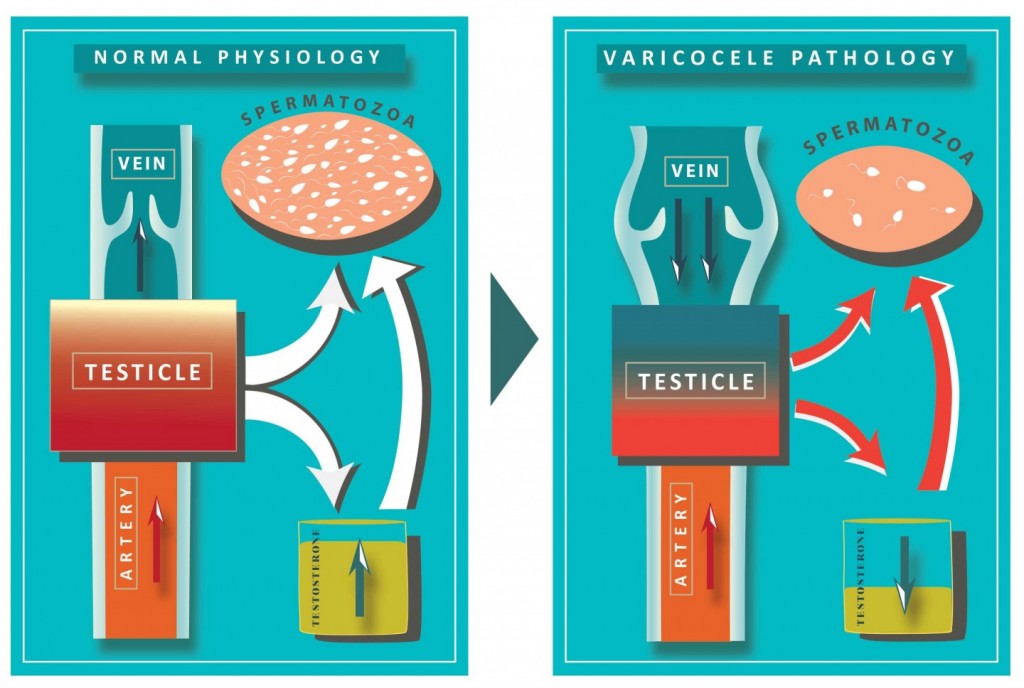
Figure 6: A. Normal venous blood flow with normal function of germ and Leydig cells with sufficient production of spermatozoids and testosterone. B. Reverse venous blood flow with increased scrotal temperature and hypo-oxygenation leading to decreased spermatozoa production and downregulation of intrinsic testosterone stimulation of spermatogenesis.
It is enough for one testicle (mainly the left) to be subject to the aforementioned chain reaction, as the following effects can also modify the other testicle’s function. There is a greater risk of varicocele occurring after puberty, especially between the ages of 15-30.
Complications of Varicocele
The main complications of varicocele are:
1. Shrinkage of the relevant testicle (atrophy): The testicle contains the tubes with the seminal epithelium, in which sperm production takes place. When these tubes are subject to deterioration due to varicocele, the testicle shrinks and becomes soft. It is not entirely clear as to why there is a shrinkage of the testicle, but the malfunction of the valve allows blood to stagnate in the seminal veins. This results in the creation of a number of factors, such as:
- Reduced delivery of oxygen to the tissues.
- Increase of oxidative stress products.
- Increased pressure on the inner tubes.
- Reduction of the intra-testicular endocrine function and endogenous regulation.
All of the above contribute towards the destruction of the seminal epithelium.
2. Infertility (sterility): Testicular veins that function normally help maintain a certain/specific low temperature in the seminal artery. This creates the optimal conditions for sperm production. When the normal blood flow is blocked, as it happens with varicocele, the temperature increases. This results in a negative effect on the level of the seminiferous epithelium. Ultimately, this leads to a reduction of the germinal epithelium’s functional capability and leads to regression.
3. Epididymal inflammatory changes: Due to the chronic temperature elevation in the epididymal tube, the storage capacity of sperm reduces. This results in decreasing of the sperm count and the quality of the ejaculate.
Tests & Diagnosis of Varicocele
Clinical examination: In the clinical physical examination, the doctor usually finds a spiral mass which is not painful when palpated. This gives the impression of a ”bag of worms” to the examining doctor and happens when it is sufficiently dilated. This usually happens in third grade varicocele. As part of the process, the patient takes a deep breath which applies a downward pressure. Thus, the already-expanded veins will become more visible which helps with the diagnosis.
Ultrasound imaging: The doctor takes ultrasound images using a special ultrasound probe of high sensitivity. This requires a urologist who is additionally specialized in ultrasonography of the urogenital system. Through this exam, the doctor can discover the existence and extent of anatomical damage to the venous plexus and the reflux dysfunction of the venous flow. This will simultaneously confirm or exclude the existence of any other possible causes that may be responsible for any discomfort in the area.
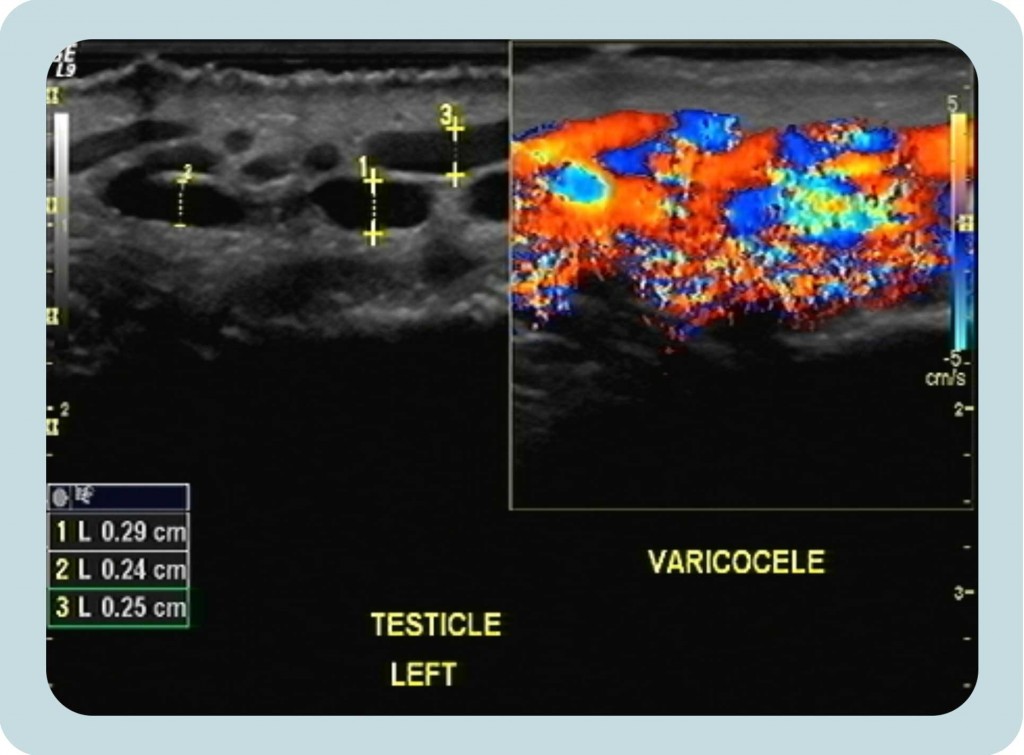
Figure 7: A. Ultrasound image which shows the dilated veins of the pampiniform plexus with diameter more than 0.20cm during the Valsalva maneuver. B. Colour Doppler image showing the reverse venous blood flow by demonstrating multiple “serpentine” vascular channels within the scrotum, which become prominent after Valsalva maneuver.
Treatments of Varicocele
Patients should treat their varicoceles when there is:
- Severe and chronic pain and medication doesn’t help.
- A testicle has been subject to shrinking (compared to the other testicle).
- Caused abnormalities in sperm resulting in the person being infertile or sterile.
- Enlargement of the varicocele to a degree that is prominently visible to the naked eye.
Although varicocele often develops at a young age, it is not completely clear when it should be operated on. Unless the aforementioned signs appear, surgery can be avoided.
Methods of surgical treatment
A. Microsurgical Varicocelectomy
This is the best option for a full recovery of varicocele. The doctor performs a small incision without section of any layers of myofascial tissue, providing prompt and excellent access to the level of the spermatic cord. The process is:
- Using the surgical microscope, the separation of individual anatomical components of the tone is absolutely clear (i.e. veins, seminal artery, lymphatic vessels, etc.).
- Then, the doctor performs careful and detailed ligation of all pathological veins.
Effectively, the doctor ties all the problematic veins, while being very careful to avoid all the healthy veins (with the lowest probability of varicocele recurrence).
Post-operation, the patient:
- Can normally return to their daily life after one day of hospital stay.
- May experience minimal pain. The doctor typically prescribes analgesic and anti-inflammatory drugs for a couple of days after the surgery.
- Will take antibiotics for a couple of days as is normal after surgeries.
- May have sexual intercourse two weeks after the surgery.
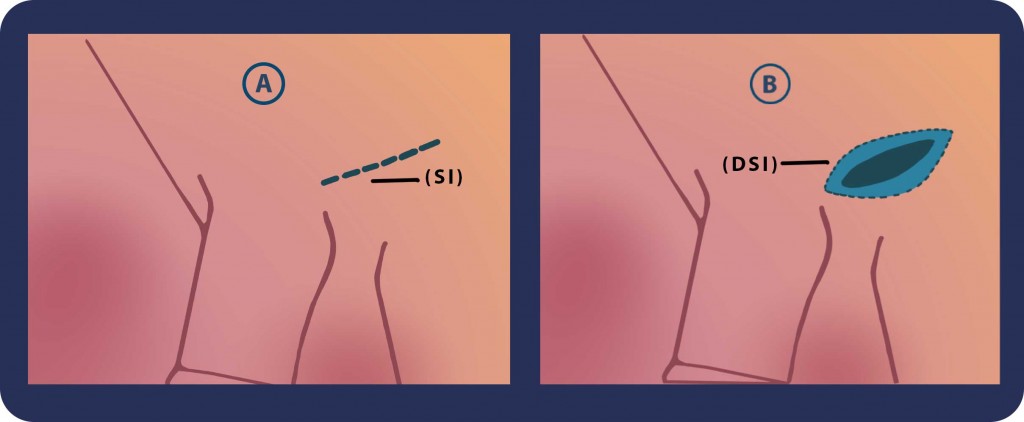
Step 1: We begin with 3-cm slightly oblique skin incision (SI) just over the external inguinal ring. The incision is deepened (DSI) through adipose tissue and Scarpa’s fascia. Then we identify the spermatic cord.
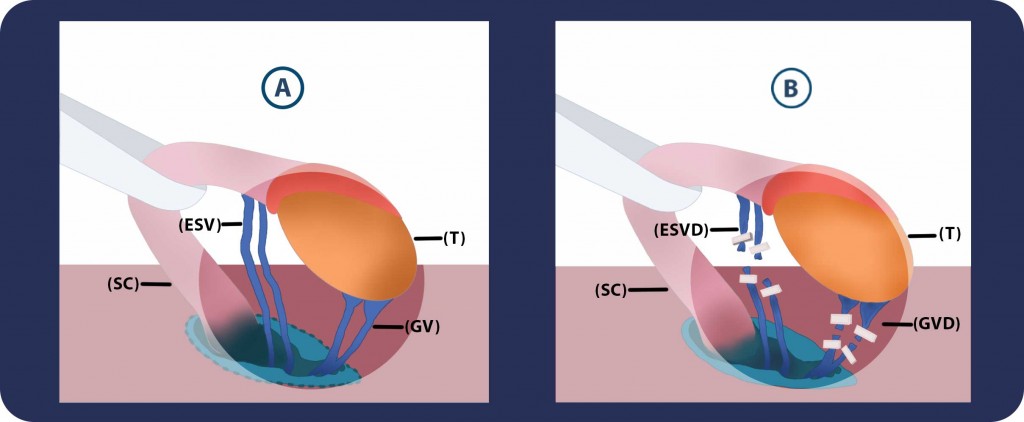
Steps 2 & 3: A.We grasp the spermatic cord (SC) and the testicle (T) with a Babcock clamp and place both of them over Penrose drain. B. Then we isolate and divide the gubernacular veins (GVD) and external spermatic perforators (ESVD).
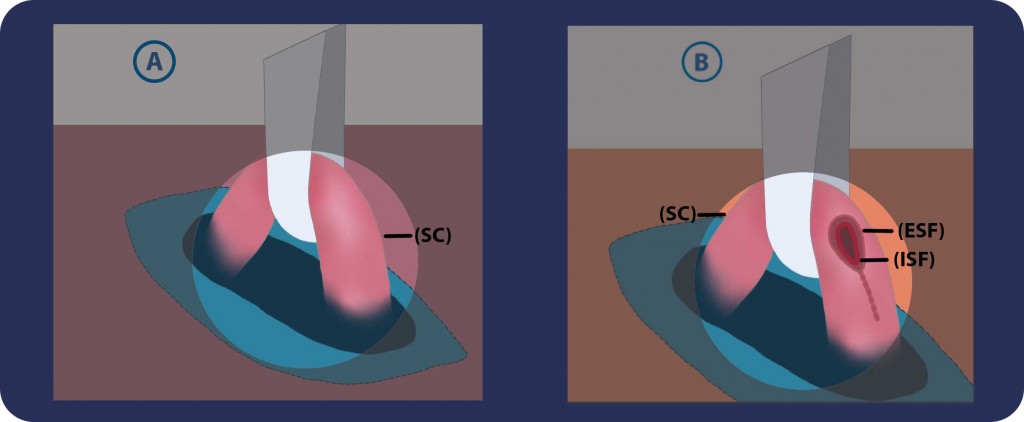
Steps 4 & 5: We first incise the external (ESF) and internal spermatic fascias (ISF) and then we examine and dissect carefully the cord (SC) structures
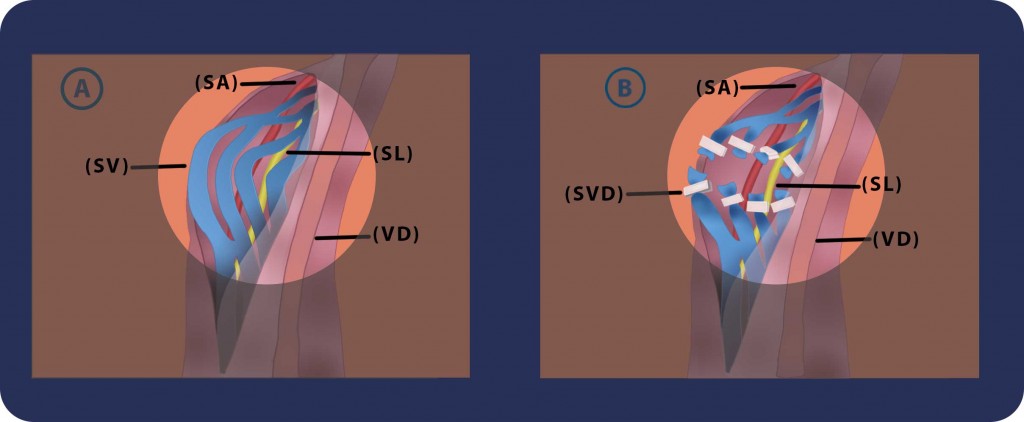
Steps 6 & 7: We identify, protect and preserve the spermatic artery (SA), vas deferens (VD) along with its vessels, the cremasteric artery and the lymphatic channels (SL). We isolate, ligate (silk ties are used and alternatively surgical clips) and cut all the spermatic veins (SVD) and the cremasteric ones. After cutting all these veins, the blood is able to leave the testicle through the veins of the Vas deferens. These veins are less likely to become swollen.
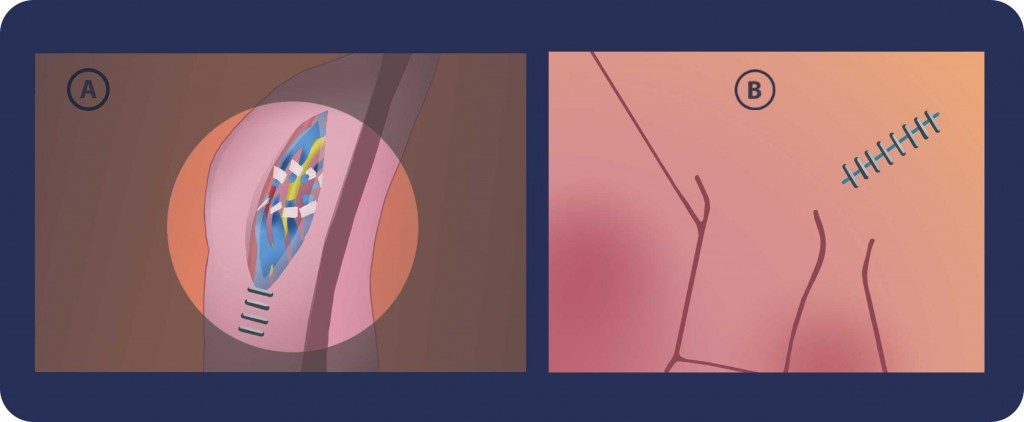
Step 8: A. We place the spermatic cord back to the skin incision. We irrigate the wound with an antibiotic solution and Scarpa’s fascia is then closed with a single chromic catgut suture. B. The incision is infiltrated with an anesthetic and the skin is closed with a running subcuticular closure.
Regeneration of the seminal line usually takes three months. The doctor additionally asks for a semen analysis after three to four months post-surgery. If necessary, the doctor assists the post-operation therapy with medication, including hormonal pills, vitamins etc.
This is the method of preference for Georgiadis Urology as it has the highest benefit (with over 98% success rate and almost non-existent cases of recurrence) and low downtime for the patient.
B. Laparoscopic & Robotic Surgery
This is a good alternative because it happens through small holes in the abdomen. This means that postoperative pain is minimal and an even faster return to daily activities. Of course, this method takes place under general anesthesia, with a minimum hospital stay (i.e. one day). The drawback is that the probability of varicocele reappearance (post-surgery) is about 8%-10%.
C. Percutaneous embolization
This method only requires local anesthesia. The process is as follows:
- With a small opening at the top of the scrotum, an enlarged venous branch of the pampiniform plexus is discovered.
- Then, small venous catheter is inserted and stabilized with sutures in the discovered vein.
- A special contrast agent is introduced through the venous catheter.
- With the help of a special X-ray, the inner sperm vein in all its course is shown due to the contrast agent.
- Finally, the embolization takes place with a special substance that hardens and clogs the vein a few minutes after its infusion.
The patient checks out of hospital on the same day, 2-3 hours after surgery. This is the best method in terms of downtime, however the reoccurrence rate can reach up to 15%.
Other surgical approaches
Many doctors operate on varicocele cases, with:
- An incision at the level of the inguinal canal (i.e. transinguinal).
- Top and sides of the inner mouth in the lower abdomen (known as the method of Palomo or retroperitoneal).
- A small incision below the inguinal resource (subinguinal).
