Chronic Cystitis – Condition
What is Chronic Cystitis?
Chronic cystitis is a long-standing inflammation that develops in the wall of the bladder. The bladder infection is primarily painful, irritating and generally impairs the quality of life. Chronic cystitis could constitute a serious health problem if the infection spreads to the kidneys and the genital system.
It is a clinical syndrome characterised by a group of symptoms which primarily include:
- Dysuria (i.e. painful urination)
- Urinary frequency
- Urinary urgency
- Low pelvic pain
- Feeling of incomplete emptying
All these can occur together or separately and they vary widely in intensity, with periods of remissions and exacerbation.
Causes of Chronic Cystitis
A. Microbial Factors
In chronic or recurrent cystitis we often have to deal with various infectious microorganisms, the most frequent of which are:
- Escherichia coli (65% to 70% cases)
- Proteus (35% cases)
- Klebsiella (30% cases)
- Enterococci (25% cases)
- Streptococcus group B (15% cases)
All the aforementioned microbes can be found as a single agent or in group of two (or even three), in urine and vaginal fluid cultures. Unfortunately, it is very often the case that the urine/vaginal microbiological tests are performed inadequately, and thus fail to uncover the agent. This is why it is so crucial to visit a specialised microbiologist.
In addition, there are other well known microorganisms which are commonly transmitted sexually (among the others) and can constitute the causing factors of cystitis, such as:
- Chlamydia (30% cases)
- Ureaplasma (25% cases)
- Mycoplasma (15% cases)
- Gardnerella vaginalis (10% cases)
These mostly (if not only) appear in vaginal cultures but can infect the urinary bladder as well.
B. Improperly Treated Bladder Pathological Conditions
Former bladder pathological situations or pelvic painful syndromes which are misdiagnosed and improperly faced, can lead to chronic bladder inflammatory disease.
The most frequent scenarios are:
- Acute urinary infections which have subsided without getting any kind of treatment or where improperly treated.
- Occult urinary infections (minimal symptoms and annoyances) which we usually attribute to other regional organs’ pathology or diseases.
- Pelvic pain with absence of microbes in the urine culture, which we often attribute to anxiety or other psychosomatic issues.
All three cases are very common, and this is why female patients should visit a urologist promptly if they experience any of the above, to prevent the problem from becoming chronic.
Important notes
- From our experience in treating chronic or recurrent cystitis, the causing factor is always microbial.
- The aforementioned infectious microorganisms are very often found simultaneously in vaginal fluids cultures.
- Regardless of if there are symptoms in the vagina, the presence of microbes in the vaginal fluid confirms the close urethral-bladder relation to the vagina.
- The other genitalia (cervix, uterus, ovarian tubes, etc.) could be infected, depending on how long the infection has existed.
- The need to deal with the infection (chronic cystitis) along with the other inflammatory sites in the urogenital system is of great importance for women overall.

Figure 1: General representation of the female urogenital system. It is shown the close relationship between urinary system (urethra – bladder) with the genital tract (vagina – uterus – fallopian tubes).
Pathophysiology of Chronic Cystitis
A. Mechanism of infection
Microbes primarily enter the urethra and invade the bladder wall. These kinds of microorganisms are in many cases similar to those microbial colonies present in the intestinal tract. We can also find them in the perineal area and in the vaginal fluid as well. To infiltrate the bladder mucosa and create inflammation, the presence only of the microbial agent is not enough. Under special circumstances and due to a variety of reasons, microbes suddenly express intense virulence properties. These properties allow the microbes to attach to and penetrate areas with easy access to the bladder such as the urethra or the vagina.
B. Mechanism of long-induced pathology
There are three theories that might explain why many women are plagued with chronic or recurrent UTIs:
- Occult or acute but improperly treated e. coli infections might reprogram the lining of the bladder, making it more susceptible.
- Bacteria can hide and remain invisible creating a cloak made by a biofilm. This is made of microorganisms that stick to each other and cover a surface, in this case the bladder wall. Thus, the antibiotics are unable to reach the bacteria, which then re-emerge when the immune system goes down.
- The microbes can enter and penetrate into the deeper layers of bladder mucosa and from those a small number could enter even into the cells of the urothelium. This intra-cellular colonization will go into a dormant state similar to hibernation for a long time. This is an important point, because the microbes inside the cells are not affected by antibiotics and cannot be perceived from the organism’s defensive mechanisms. The microbes can be activated at any moment, dividing themselves and penetrating into the new fresh cells of the urothelium.
C. Compromised defensive mechanisms
Quality of urination: A very good stream, where there no urine residue, is an important factor which prevents a possible infection. In the opposite case, where the urination becomes compromised, the situation favours the establishment of infections. This happens in cases such as:
- Dysfunctions of the bladder-urethral mechanism
- Urethral strictures
- Urethral prolapses
Defensive urethral cell lines: The existence of defensive cell lines along the urethra, intercept and capture incoming microorganisms. In cases where we have injuries or inflammations in the urethra, it is understood that the mechanism’s effectiveness wanes.
Vaginal mucosal defense: The vaginal mucosal layer and perineal area have microorganisms such as lactobacilli as well as acidic micro-environments, as defensive mechanisms. These inhibit the attachment of various germs. There are situations that might change the micro-environment of the vaginal wall or the perineal area such as:
- Fungal infections
- Use of various antibiotics
- Drugs or other medicines
- Vaginal atrophy
All of the above will reduce the resistance locally and could create conditions which will favour infections such as chronic cystitis.
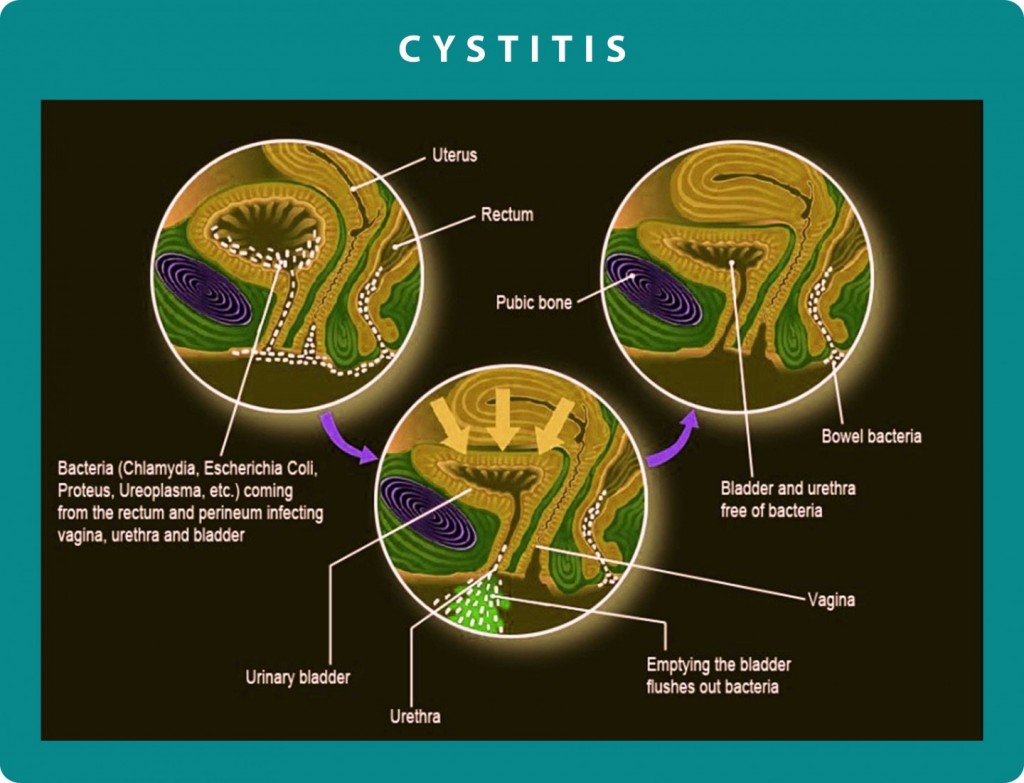
Figure 2: In this image we can see the migration path of bacteria from the intestine and the perineal area to the vaginal cavity and bladder. We can also see the direct anatomical relationship of the vaginal cavity to the bladder which justifies the fact that when the one cavity is infected, the infection is quite easily expanded in the other one too.
D. Predisposing factors of chronic cystitis
There are a number of factors that can contribute to chronic cystitis:
- The length of the female urethra is 4 cm (unlike in men which is 15 cm) – this means the distance for a microbe is shorter.
- The vaginal contraceptive diaphragms (for younger women).
- Frequent sexual intercourse, especially when precautions are not taken.
- Frequent use of antimicrobial drugs which have the side effect of reduction or destruction of the normal flora. This results in changing of the micro-environment in vaginal or perineal area, making it more vulnerable.
- Nutrition with excessive consumption of alcohol and sugary foods.
- Hormonal abnormalities such as the drop in estrogen may lead to changes in the homeostasis of tissues. In the vagina, urethra and bladder the tissue becomes thinner, weaker and loses the protective layer. All these changes increase the risk of infection or relapse of the inflammation.
- During pregnancy, the changes that occur in the urinary tract increase the rate of infections (such as chronic cystitis).
- For women with more than two births or women at a slightly older age (or after menopause), problems such as:
- Urinary incontinence
- Cystocele
- Atrophic Vaginitis
- Urinary tract infections
