Chronic Prostatitis – Symptoms
What are the symptoms of Chronic Prostatitis?
Many patients remain undiagnosed for years despite regular visits to their urologist. Some may even think they have no problem as the symptoms may remain subtle for a long time. Correctly understanding the symptoms is absolutely critical to treating the condition and saving lives. After 25 years dealing with a vast number of patients of all ages, I have become used to spotting the persistent warning signs of chronic prostatitis whether they occur individually or simultaneously.
Erectile & Sexual Dysfunction: A decrease in sexual desire can be an indicator of chronic prostatitis. Morning erections may become less frequent or fail to reach the usual hardness. Evoked erections may also become less hard. Even if erections reach the desired hardness initially, it is subsequently lost during intercourse or undergo instantaneous transitions. Due to the complexity of erectile dysfunction, we have dedicated posts that explain its correlation with chronic prostatitis and its treatment.
Changes in the frequency of urination / micturition: Chronic prostatitis gradually increases the frequency of urination from 3-4 times per day to 6-8+ times. Over time it becomes a habit rather than feels like a symptom. In addition, the average nighttime frequency (nocturia symptom) can increase from zero to once or even 4 or 5 times.
Reduced urination power / flow: The radius of the urination begins to decrease, gradually losing its natural curve until, in many cases, the patient ends up pressing the belly to boost or even accomplish urination.
Feeling of incomplete emptying of the bladder: The patient feels that urine remains in the bladder, often creating the sensation of a need for a second urination after a short while.
Urination Hesitancy: The patient feels that they want need to urinate, they go to the toilet but urination does not start immediately. There is a short amount of waiting time before the urination begins.
Post-void Dribbling: This happens when men involuntarily lose a small quantity of urine shortly after they have left the toilet. Patients report that this is one of the most annoying symptoms, as it wets their underwear. Even if patients wait after urination and gently shake the penis, the problem still remains.
Infertility / Difficulty in conceiving: When the examination results of the female partner are normal, semen appears to be responsible for 50%-60% of cases where couples have difficulty in conceiving (i.e. male infertility). The toxic effect of chronic inflammation drastically reduces the sperm count and sperm mobility. In many circumstances chronic prostatitis coexists with varicocele(s) which may result in the dysfunction of sperm, but the main cause remains the chronic inflammation of the prostate.
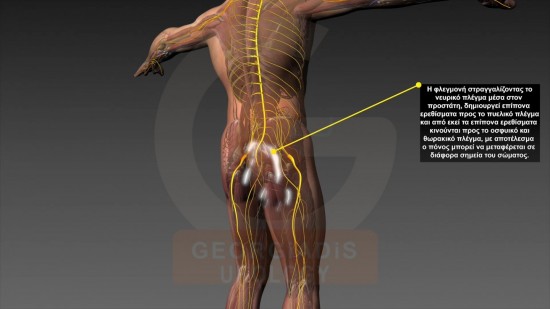
Nerve strangulation: There is a variety of effects due to the intraprostatic tissue fibrosis on the nerves such as:
- Sensation of heaviness or numbness: Heaviness, numbness or even pain in the lower abdomen, the groin and/or over the genitals.
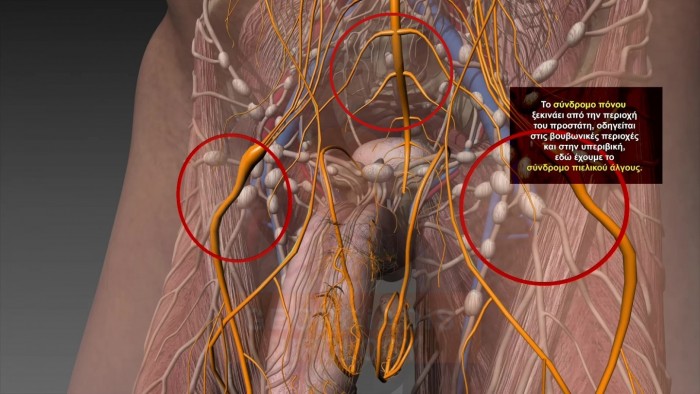
Figure 1: Visual representation of the reflections of the pain which originates from the strangulated intraprostatic neural network towards the lower abdomen and the groin. Due to these symptoms, many doctors often misdiagnose Chronic Prostatitis as Pelvic Pain Syndrome and as such they treat it as a muscular condition. The matter of the fact is that this is nothing other than a symptom of Chronic Prostatitis rather than a the disease by itself.
- Pain, sense of burning or numbness in one or both testicles and/or penis: Problems in the veins of the testes (varicoceles) can complicate the diagnosis. Continued pain in the testicles even after surgical treatment is a strong indication of chronic prostatitis.

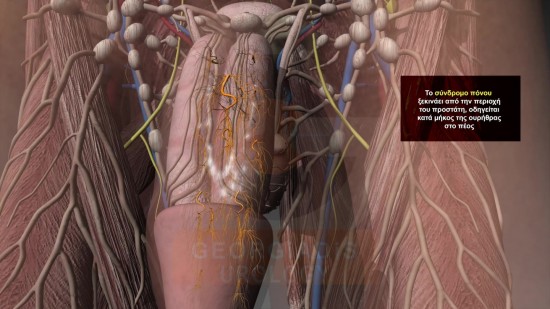
Figures 2 & 3: Visual representation of the reflections of the pain which originates from the strangulated intraprostatic neural network towards the testicles and the penis.
- Feeling of burden or pain in the lumbar or lower spine: Many patients have needlessly undergone CT and MRI examinations and even clinical interventions for false diagnoses such as hollow intervertebral disc or kidney lithiasis (stones) when in fact they suffer from chronic prostatitis.
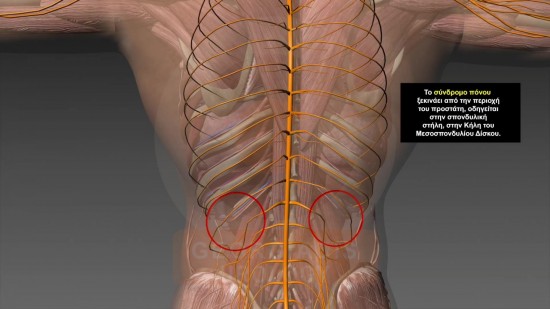
Figures 4 & 5: Visual representation of the reflections of the pain which originates from the strangulated intraprostatic neural network towards the lumbar and/or lower spine. This is also one of the symptoms that often causes doctors to misdiagnose Chronic Prostatitis Symptoms with the Pelvic Pain Syndrome but also with hernia of lumbar spine.
- Feeling of rapid fatigue: In more than a few cases patients suffering from extreme fatigue due chronic prostatitis have undergone a plethora of clinical and biochemical examinations without being able to find the root cause.
- Pelvic pain and/or feeling of fatigue or pain in the thighs: Tiredness, pain or grip in the pelvis or the thighs which is not justified by the daily workload. The pelvic pains are often sharp as if something is stabbing or severely clamping the area, whereas the thighs feel severe tiredness.
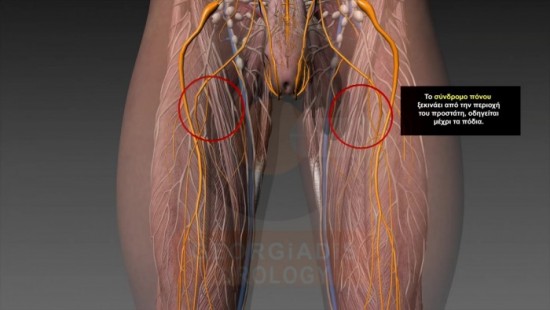
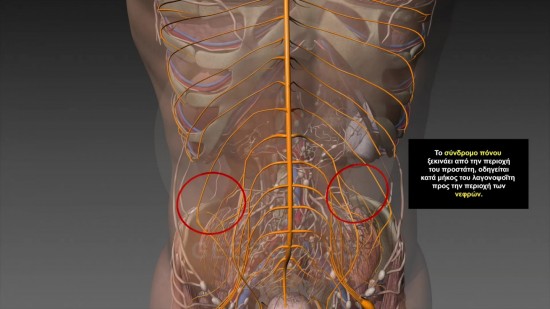
Figures 6 & 7: Visual representation of the reflections of the pain which originates from the strangulated intraprostatic neural network towards the pelvis and the thighs.
- Vertigo, headaches or cervical pain: Vertigo, headaches or cervical pain with remissions and aggravations where clear causes are not identified by standard tests.
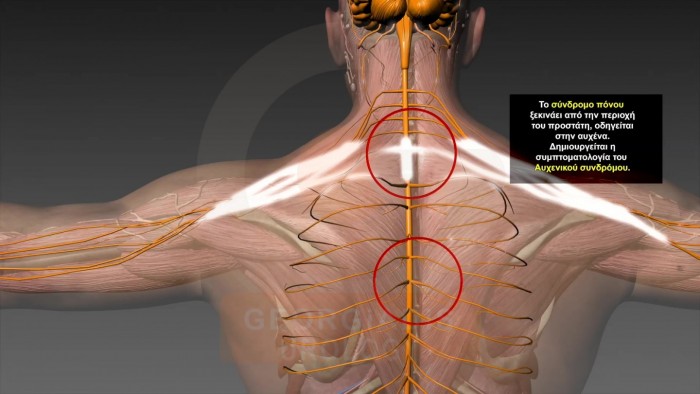
Figures 8: Visual representation of the reflections of the pain which originates from the strangulated intraprostatic neural network towards the cervical area. Sometimes the pain is reflected all the way to the hands as well as the head.
Prostatitis Signs
Light and periodical burning sensation in the urethra or the head of the penis during or even outside urination: In some cases, the burning pain in the perineal area or along the penis is very strong and almost unbearable, particularly after spending hours sat on a bicycle, motorbike or car seat.
Balanoposthitis: Inflammation of the glans and the prepuce of the penis (usually with a fungal cause) that do not subside after treatment.
Acute Epididymitis: Painful and swollen semi-scrotum, with testicular pain and tenderness, high sensitivity on touch and potentially associated with discomfort in the lower abdomen and ocassionally fever.
Chronic Occult Epididymitis: This refers to a small swelling of the epididymis with a very vague feeling of heaviness. It is named medically occult as it does not exhibit obvious symptoms, but it is often co-occuring with chronic prostatitis. This creates problems in sperm transporation due to blockages in the efferent ducts of the epididymis, ultimately contributing in male infertility.
Changes to the time of ejaculation: Premature or delayed ejaculation may both be symptoms of chronic prostatitis.
Burning penile sensation: Pain or burning during or immediately after the ejaculation. This happens from the base of the penis and can be felt all the way to the glans.
Haematospermia: Appearance of dark brown semen or even blood in the semen, with periods of remission and exacerbation.
Hematuria (Blood in Urine): Appearance of blood in the urine due to the chronic prostate inflammation, which causes friability of the small tissue vessels. For more information please refer to the dedicated hematuria page.
Change of defecation habits: In a few cases, the chronic inflammation of the prostate is associated with intense constipation. Due to its common innervation with the gastrointestinal system, the affected urogenital system can create serious problems with defecation.
Appearance of blood in faeces: Haemorrhoids often coexist and are intensified by chronic inflammation of the prostate.
Outflow of synovial fluid: An unusually pale, slightly turbid or even sometimes purulent fluid may be observed. This is caused by the pressure applied to faecal matter as it passes through the intestine onto the inflamed prostate.
Reoccurring urinary tract infections or acute prostatitis: In some cases, patients have previously undergone treatment for acute prostatitis as (mis)diagnosed by their urologists often multiple times, after which their symptoms largely subsided. Years later when visiting my clinic, tests in 90% of cases reveal that these acute inflammatory situations were actually symptoms of chronic inflammations of the prostate gland that had obviously not been properly cured.
Late Complications
Prostate hyperplasia: Chronic prostatitis can be considered as the pathogenic background for the increased cell multiplication in various cellular pathways (i.e. hyperplasia) as well as the increased cell size (i.e. hypertrophy). This effect is possibly a consequence of the autoimmune reaction mechanism against auto-antigens released after the damage caused by inflammation, oxidative stress and hypoxia in the prostate tissue.
Adenocarcinoma: There is research, based on epidemiological, anatomical, histological, molecular and genetic data, that suggests a correlation between chronic inflammatory disease of the prostate with the development of prostate cancer. While the research is non-conclusive, this correlation can also not be disputed. This is because no one can claim that a prolonged condition (i.e. chronic prostatitis) that affects the prostate cells and causes proliferative inflammatory atrophy (which is considered precancerous lesions) is uncorrelated with prostate cancer. Older men with very chronic prostate inflammations should be aware of this possibility. It is not a random event after all, that one of the most stastistically common forms of cancer is prostate cancer.
