Chronic Cystitis – Therapy
How to treat Chronic Cystitis?
Medication
The first step in treating cystitis is to organise the appropriate medication. This typically means using a combination of therapeutic substances and in order to make the right selection, we need to keep the following in mind:
- Detected microbes: Detected microbes and their resistances are critical in antibiotics selection, but it is important to keep in mind that not all of the microorganisms can be identified in early urine and vaginal fluid cultures. This means that sometimes we may have to account for potential microbes that may not be visible in the urine or vaginal fluid cultures.
- Severity of lesions: The severity of lesions detected in the urethra, bladder, vagina, cervix and uterus.
- Complications: The existence of complications accompanying the inflammations (urethral stricture or malfunctions in the urination mechanism).
- Chronicity: The chronicity of the inflammations depending on the patient’s history.
The conservative medication duration can last from 1 to 3 months, with some cases needing further treatment (e.g. up to 9 months). In addition to the antimicrobial therapy to combat chronic cystitis, we can use medicines that are related to the reduction of some intensive symptoms. These are meant to decrease discomfort such as frequent and urgent urination.
Georgiadis Chronic Cystitis Protocol (GCCP)
Intravesical Instillations Therapy
Intravesical instillations are a necessity in most cases of chronic cystitis and a core part of the Georgiadis Chronic Cystitis Protocol. The long-standing bladder lesions are highly resistant to treatment solely based on oral medications. The use of specific medicinal substances in mixtures at appropriate concentrations has proven to have extremely good therapeutic effects. This approach significantly improves or even completely cures chronic cystitis in many cases. It is effective even to the most difficult situations of persistent and extremely annoying for the everyday life symptoms.
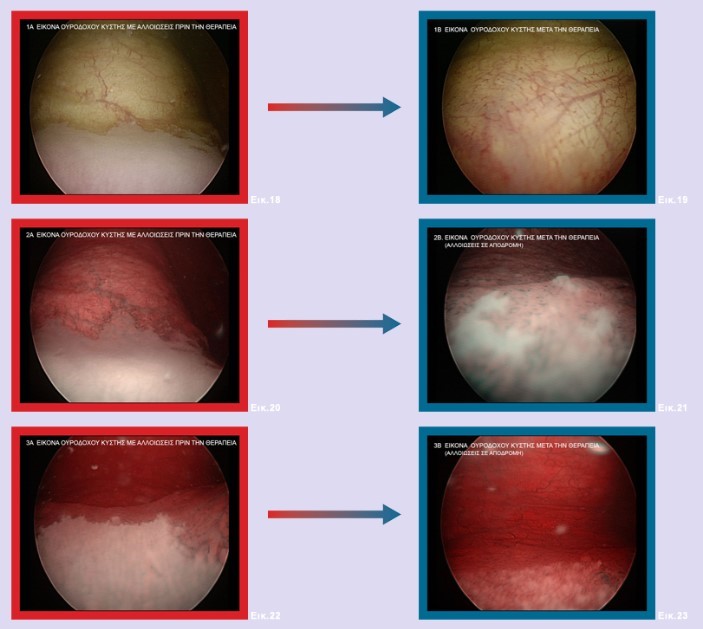
Figure 1: Chronic membranous cystitis in resolution after a series of intravesical infusions.
The intravesical therapy is an easy and painless method which is achieved by the input of a narrow band disposable catheter into the bladder, through which the pharmaceutical mixture is injected. The drugs should remain in the bladder for about two (2) hours and then be removed naturally by urinating. The results of the intravesical therapy are considered absolutely positive in percentage more than 92% of all patients. Their application frequency varies according to the intravesical lesions.
The Georgiadis Chronic Cystitis Protocol (GCCP) typically consists of:
- First stage: The frequency of antibiotic instillations is typically three per week, but it can be lower or higher depending on the patient’s condition and usually lasts for 1-2 months.
- Second stage: We perform a few instillations every month, for three to six months.
Intravaginal treatment
The coexistence of a microbial infection in the vagina is very common (rates exceeding 70%) and should be treated simultaneously with cystitis. In case it doesn’t recede with the usual oral medication, intravaginal ointments are applied, which are effectively mixtures of appropriate antibiotic vaginal creams. Thus, we achieve increased concentrations of drug in the vaginal area and uterus, especially in cases where the germs have penetrated there too.
Urethral Dilations
We perform urethral dilations in the cases of coexistent urethral stricture as functional or organic complication of the chronic inflammation of the urethra and bladder. The stricture (after its formation), makes the disease very difficult to cure, if it is not recognised and treated in time. The urethral dilations are conservative surgical interventions using local anesthesia and are very well tolerated by patients with chronic cystitis.
Transurethral endoscopic electrocautery
There are some very difficult cases (which are about 10%-15% of cases) which are very chronic and have lesions that are highly resistant to intravesical infusions. In these cases, we recourse to the cauterization of the lesions, simultaneously with the antimicrobial treatment. This is accomplished by using the transurethral electrocautery device. As an alternative solution we can use the neodymium (Nd):YAG laser. The healing results are very encouraging, especially after an initial treatment with intravesical instillations. The cure rate is almost 96% of all patients suffering from chronic cystitis, about three months after the operation.
Immunoprophylaxis
Using antimicrobial vaccines, there is a small number of patients with moderate improvement. This improvement manifests itself in two ways:
- Slight decrease in the strength of the ailments.
- Increase of the interval between the recessionary phases of the disease.
In our experience, patients who go through this do not remain satisfied since the symptoms remain in a significantly disturbing extent. Even after the continuous intake of the pharmaceutical package for a long time, the prophylactic outcome remains poor. Thus, it can be used or suggested by some gynaecologists or urologists, but the results do not seem to justify their use.
Chemoprevention
Chemoprevention refers to taking antimicrobial drugs in small doses for very long periods of time in order to:
- Maintain a state of remission.
- Lower intensity of the symptoms.
- Prevent the frequent occurrence of periods of exacerbation of the disease.
Chemoprevention does not seem to produce the expected results in the management of chronic cystitis. In most cases, especially in patients with an extended history (at least over 2-3 years), it does not bring any practical effect.
On the contrary, we would say that it probably results in negative effects such as:
- Partially covering the symptoms, which may reduce the urgency to treat the disease.
- The development and progressive burden of inflammation is not inhibited, but may be masked.
- The expansion of damage and its complications if the package is not appropriate.
- Microbes gaining reactive resistance, making them persistent even against the most powerful antibiotics.
- Overall strain on the body.
This is something we come across with a significant number of patients. Before coming to us, they typically have received different treatments either of chemoprevention or with powerful antibiotics, for several years (e.g. 6-10 years). Their intention is usually to cope with recurrent acute inflammatory conditions (e.g. recurrent UTIs) or other symptoms of chronic cystitis, or because they found a microorganisms such as:
- Enterococci
- Staphylococci
- E. coli
- Proteus
- Klebsiella
- Chlamydia
Unfortunately, this course of action leads to rendering those organisms very resistant even to the most powerful antibiotics. These patients would eventually come to us to be radically treated, but of course due to the resistance of the microbes, more time is needed until the final recovery, resulting in additional psychological burden. As such, we would strongly urge patients to be very critical before accepting any antibiotics-based treatments and to only visit urologists with successful track records in treating cystitis.
