Chronic Prostatitis – Condition
What is Chronic Prostatitis?
Chronic prostatitis is the end result of a series of inflammatory reactions in the prostate gland that in turn affect the entire genitourinary system.
These reactions are caused by a variety of germs including coliforms, enterococci, staphylococci and the proteus, in addition to a number of microorganisms including chlamydia, ureaplasma and mycoplasma.
Other microorganisms as yet unidentified by modern microbiology may also play a part. These can only be detected by an electron microscopy in the cultures of the expressed prostatic fluid and semen.
So, the root cause in the overwhelming majority of chronic prostatitis cases is microbial.
The distinction between bacterial and non-bacterial chronic prostatitis is defined by the presence of a microbial agent in the cultures of prostatic fluid / semen. However, even If bacteria are not discovered in the initial examinations, it does not mean that it is truly non-bacterial.
In both cases, the existence of leukocytes indicates an inflammation and both cases (bacterial and non-bacterial) can be controlled by use of antibiotics, regardless of course if the antibiotic alone does not lead to a radical result.
The percentage of the male population affected
- Recent studies indicate that 65% – 70% of the male population suffer chronic inflammation lesions in the prostate tissue. Post-surgery histological tests for hyperplasia / hypertrophy of the prostate and prostate cancer reinforce this data.
- The particularly high rate of chronic inflammatory lesions in surgical specimens of hypertrophy or prostate cancer indicates a causal relationship between chronic inflammation with hyperplasia of prostate tissue and the potential for cancerous growth.
- This is crucially important because it necessitates the rapid and radical treatment of a disease which plagues the older part of the male population above all.
Approximately 50% of males will show symptoms related to chronic inflammation at some point in their lives.
- A large percentage of males aged 20-35 will show irritative symptoms e.g. pelvic pain, burning sensation on urination, sense of weight in testicles etc.
- A large proportion of males aged 35-55 will show more obstructive symptoms e.g. varying degrees of dysuria with almost guaranteed evolution of chronic prostatitis and an enlarged prostate gland.
- Further complications exist in both age groups e.g. erectile dysfunction, sub-fertile sperm and so on.
- Symptoms depend on the speed at which the inflammatory lesions evolve and spread in the prostate tissue; the type and quantity of microbes in the prostate; the precise area affected; and the effectiveness of the protective mechanisms in the tissue gland.
Practically speaking, we are dealing with three groups of patients.
Group 1: Urgent cases
This group experiences various intense and persistent symptoms of the chronic prostate inflammation. They typically attempt to seek immediate treatment, often looking desperately for a radical solution because of the degree to which the condition has impacted on their quality of life.
Group 2: Moderate
This group suffers periodic and moderate symptoms annoying enough to eventually warrant a visit to a urologist. Inadequate and often incorrect assessments, however, lead to ineffective treatment. Persuaded that no satisfactory cure exists, they accept that somehow this situation is the new normal. As their condition deteriorates, however, they begin to look for more radical prostatitis treatment.
Group 3: Self-denial
This group does not recognise or do not want to pay special attention to various small or moderate symptoms which begin to occur progressively. Many will undergo surgery sooner or later, either for hyperplasia or prostate cancer, because the condition was not treated properly or in good time.
At this point I must emphasise the irresponsibility of urologists who do not consider chronic prostatitis or even swelling / hyperplasia of the prostate as immediate issues to address. Instead, they regard the issue as a ‘natural’ problem to be treated only when the situation has reached an impasse – i.e. when the patient has difficulty or is unable to urinate due to an excessive swelling of the gland or the growth of cancer.
What changes occur in the prostate tissue?
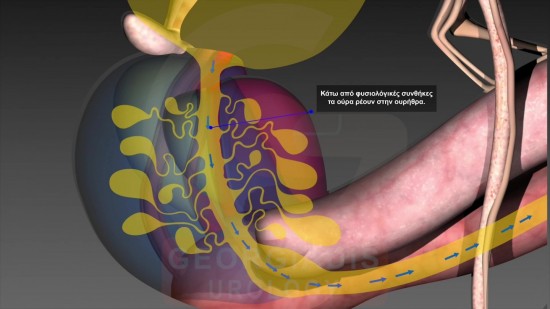
The urethra is the main microbial gateway. The first areas to be infected are the prostate glands near the urethra before the microbial infection spreads to the peripheral glands.
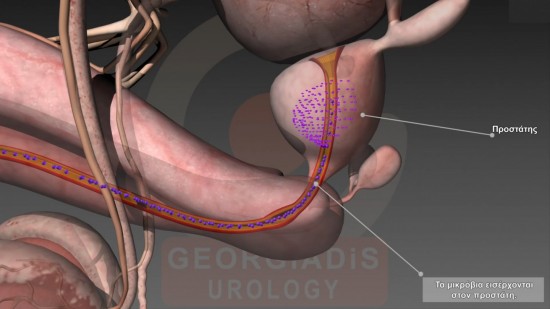
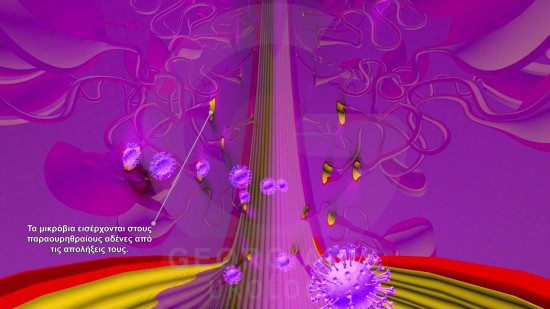
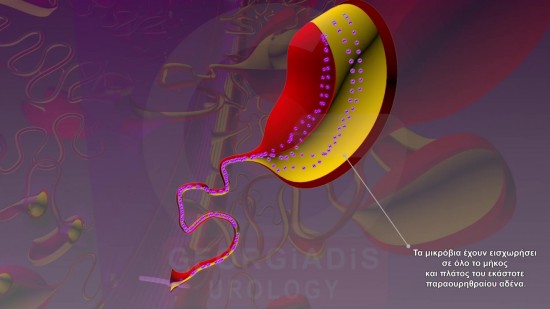
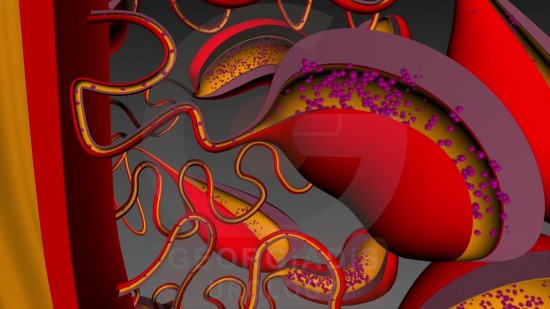
Figures 1, 2, 3 & 4: Visual representation (from upper left to lower right) of the infection stages of the prostate. 1) Initially the microbes enter the urethra towards the prostate. 2) The microbes then enter the paraurethral prostatic ducts. 3 & 4) The microbes eventually fully invade the prostatic glands.
This will be followed by clogging, a hardening of prostatic glandular tubes and the spread of the condition around the glands due to stromal inflammation and fibrosis. The hardening of the stromal tissue leads to the strangulation of blood vessels, edema and the degeneration of nerves, resulting in a lack of oxygenation and an increase in tissue oxidative stress.
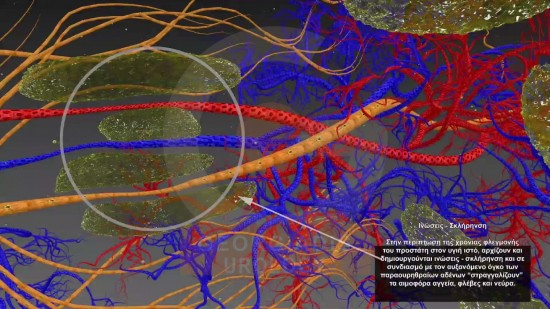
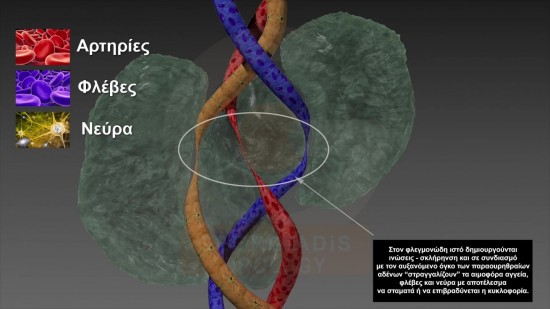
Figures 5 & 6: Visual representation of the effect of chronic prostatitis on the nerves and vessels inside the prostate (veins in blue, arteries in red and nerves in yellow). As we can see, the intraprostatic sclerosis-fibrosis leads to the strangulation of the intraprostatic neural network and vessels, which in turn results in various prominent symptoms such as erectile dysfunction, pelvic pain syndrome (and its derivative symptoms) and various micro-circulation oxygen supplying issues.
The microbes progressively generate a protective wall, multiply uncontrollably, and slowly expand throughout the prostate tissue. At this point, neither the body nor antibiotics can halt the spread.
The two events progressing around the urethra
Event 1
Small inflammatory lesions are forming alongside scar tissue causing an intraluminal narrowing at the level of the bladder’s neck or at the prostate part of the urethra (before the sphincter mechanism).
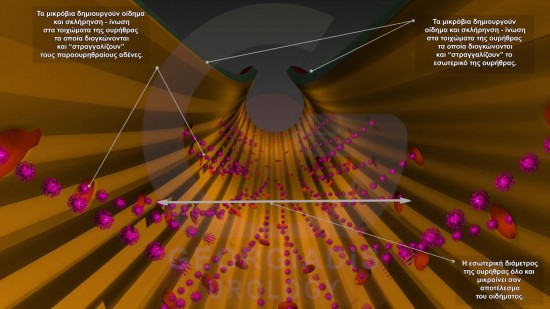
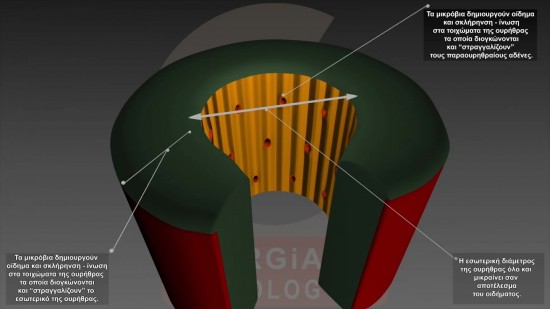
Figures 7 & 8: Intraurethral-intraprostatic reflux of urine enabling the transfer of microbes inside the intraprostatic glandular ducts. As a result of the relux, the urethral wall (represented in green in the second image) thickens and the diameter of the urethra (represented in yellow internally of the wall) is shrinking, which in turn makes the urethra more prone to the reflux effect which caused this change in the first place.
Event 2
The periurethral is hardening along the urethra prostatic part.
This in turn leads to the intraurethral / intraprostatic reflux of urine into the prostatic tubules, resulting in their calcification and the further chronicity of the inflammation.
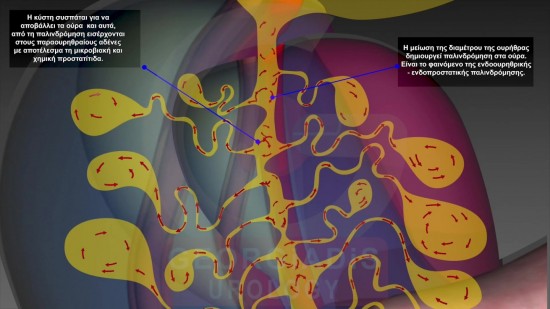
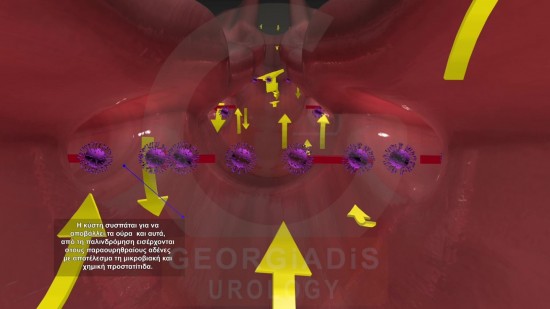
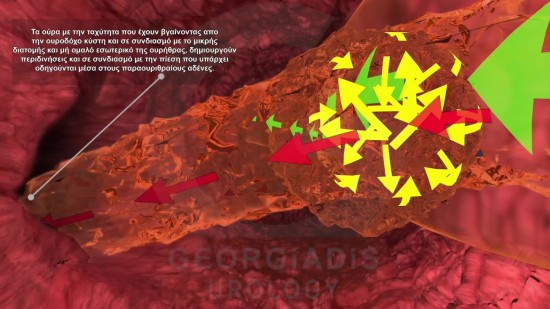
Figures 9, 10, 11 & 12: Visual representation (from upper left to lower right) of the urethral thickening and stricture effect with intraprostatic urine reflux along with the microbes. As we can see, the first effect is the edema, which is followed by urethral thickening and deformation, along with shrinking of internal diameter of the urethral lumen. This causes urine and microbes to enter the parurethral glandular ducts which in turn causes fibrosis around the urethral and further worsens the condition.
In most cases where the inflammation has caused significant chronic tissue damage, antimicrobial treatment will be unable to address the inflammation effectively. At best, the anti-inflammatory properties of antibiotics will achieve a temporary reduction of tissue edema in the prostate before the temporary masking effects wears off, revealing many more complications.
Side effects and complications of chronic prostate inflammation.
Nearly 70% of chronic prostate inflammation cases seen in urological surgeries are accompanied by side effects such as:
- Functional or organic urethral stricture: This entails varying degrees of difficulty in urinating and usually the severity of their stage is not be perceived by the patients themselves.
- Sperm infertility: The toxic effect of the inflammation causes problems in the production and quality of sperm (reduced sperm amount or low mobility).
- Erectile dysfunction: The spread of the inflammation in the erectile nerve area creates problems in inducing and maintaining the erection mechanism.
- Increased prostate size: Continuous inflammation induces hyperplasia and hypertrophy of the prostate gland cells, increasing the difficulties in urinating and erection.
- Increased likelihood of tumour tissue: Continuous inflammation combined with the simultaneous weakening of the immunological mechanism (usually after the age of 60-65) increases the likelihood of tumour cells.
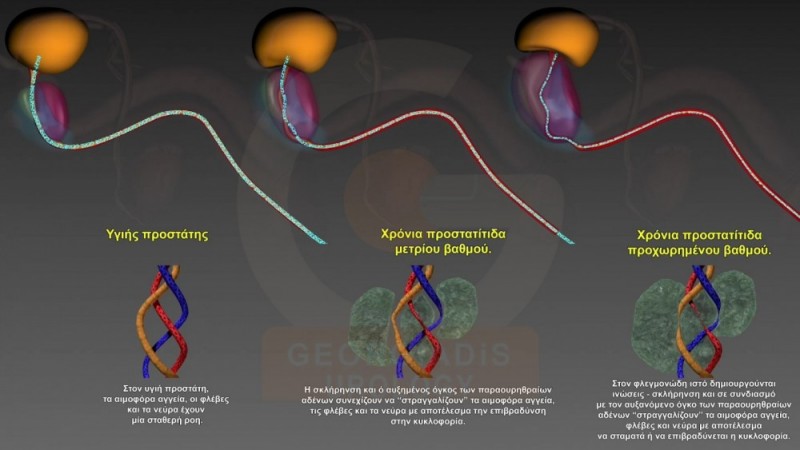
Figure 13: During the stages of Chronic Prostatitis (from left to right), the prostatic volume is progressively increasing and the intraprostatic sclerotic-fibrotic changes become more and more noticeable along with the symptoms.
