Chronic Cystitis – Diagnosis
How to diagnose Chronic Cystitis?
In the previous section we presented the range of symptoms that might indicate the existence of cystitis. In order to further investigate and objectively evaluate the condition, a doctor should perform a number of tests:
- Laboratory tests
- Ultrasound imaging
- Radiologic imaging
- Flowmetry
A. Laboratory tests
Microscopic Urine Exam
As the name suggests, the doctor examines a urine sample using a microscope. Some of the things that the doctor looks out for are:
- White blood cells
- Red blood cells
- Bacteria
- Crystals
All the above findings of microscopy are strong indicators for the diagnosis of Urinary Bladder Infection.
Urine dipstick test
A urine dipstick test can check for the following:
- Acidity (pH): If the acidity is abnormal, the patient could have a urinary tract infection (UTI) or another condition.
- Protein levels: This could be a sign of infection or kidney disease.
- Glucose levels: A sugar presence indicates diabetes. Patients who fail to control their sugar level are prone to UTIs.
- White blood cells: These indicate an infection or inflammation, anywhere along the urinary tract.
- Nitrites: This would indicate presence of infection with certain kinds of bacteria.
- Red blood cells: This could constitute a sign of infection, stone or neoplastic illnesses.
A dipstick urine test with both leukocyte and nitrite-positive results is a good indication of UTI. A negative dipstick test for both leukocytes and nitrites is also useful for excluding diseases. However, many dipstick results may show single positive results, which is less helpful for drawing solid conclusions.
Urine Culture
Urine cultures are of great importance for patients:
- Who are likely to have complicated UTIs.
- With frequent reappearance of urinary problems.
- Whose initial antimicrobial therapy has failed to solve the problem.
- With atypical pelvic symptoms.
- With upper UTIs, including acute pyelonephritis.
We used to believe that the cut-off for a positive urine culture is > 100,000 cfu/mL, but this notion has changed. In the last few years, we consider that for the women with both 1) leukocytes in the microscopic urine examination and 2) urinary tract infection symptoms, a urine culture is considered positive even if the bacterial count barely exceeds 100 cfu/mL.
Important notes
- Studies have shown that over one half of patients with negative urine cultures but with a) typical UTI symptoms, b) white blood cells in the culture, had Chlamydia trachomatis.
- The remainder of women who did not have any identifiable organism, would still respond to standard therapy for acute cystitis.
- There are few cases, perhaps not more than 20%, where the microbial agent can emerge in the urine culture, and this usually happens when moderate or severe urinary symptoms coexist.
Vaginal fluid culture
The vagina is a relatively easy environment for microbial colonisation, depending on the microbe of course. In addition to local inflammation, the microbes can easily enter the urethra and the bladder. Finding the bacteria in the vagina often leads to the determination of the causative agent of chronic cystitis. We should emphasise here that performing vaginal fluid cultures correctly requires specialised skills, knowledge and experience.
There are specific evaluation protocols that must be exercised by the microbiologists. In my experience so far, many of the vaginal fluid culture results from unspecialised microbiologists are ranging from partly to completely untrue.
Important empirical notes
- There is a high possibility that the microbes we find in vaginal cultures are the causative agents of chronic cystitis.
- Vaginitis (with or no symptoms) most of the cases if not always, coexists with bladder infection.
- Chronic vaginal infection is usually expressed with recurrent fungal infection.
- Both the collection of vaginal samples for cultures as well as the culture itself, demand highly qualified and experienced doctors.
- Treatment options must always include both, vagina and bladder.
Menstrual Endometrium tissue culture
This is a very important and necessary test to show whether microbes have entered the endometrium. It is quite informative, especially when the vaginal fluid culture shows intense inflammation. Regardless of finding the microbial causative agent, even learning the number of white blood cells in the area is of great interest. From my own experience a severe inflammation of the vagina, strongly associates an inflammatory endometrium. In more than 30% of cases, vaginal infection is indicative for simultaneous existence of microbial agents in the endometrium or even at the Fallopian tubes. This situation requires in most cases, in addition to the standard oral treatment, special medical treatment (i.e. intravenous delivery of the drugs). The treatment mandates the eradication of the microbial agents from the endometrium.
Important notes
- Microbial persistence can constitute a reason for an early termination of pregnancy, especially during the first two months.
- In my experience, one of the most frequent microbial agents found in endometrial samples is Chlamydia. The microbe has been typically found responsible in cases where a huge number of efforts for pregnancy through IVF were unsuccessful (and there was no other obvious reason).
B. Ultrasound imaging
Ultrasound of Kidney-Bladder
In the hands of doctors who know exactly what they should assess from the urogenital system, the ultrasound is a valuable tool. It can show many elements that coexist or are side effects of chronic cystitis. Through this test, we evaluate:
- The functional bladder capacity.
- Residual urine amounts.
- Hypertrophy or lesions of the bladder wall.
- The existence of potential intramural lesions (e.g. tumour).
- Malfunctions of the urination mechanism.
- Kidney stones or pyelocaliceal dilatations.
- Ureterovesical junction (UVJ) stones / obstruction.
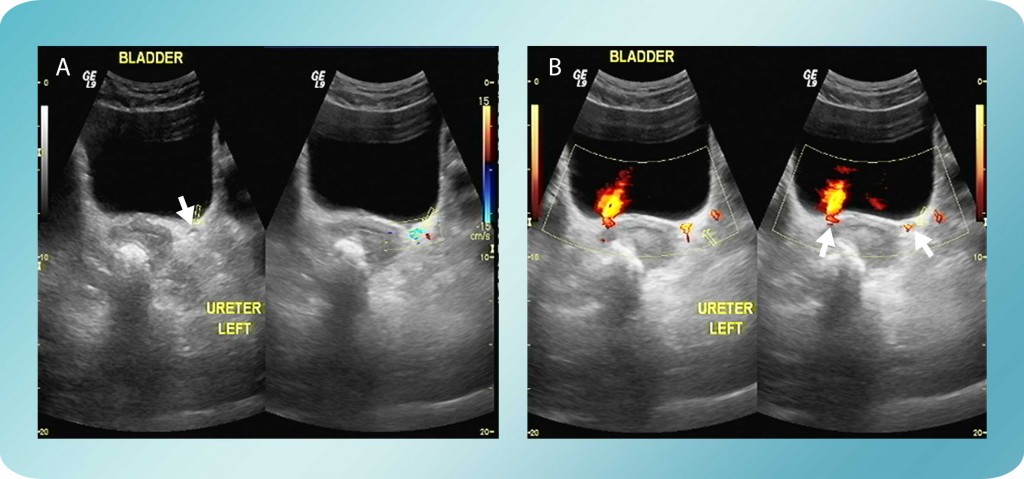
Figure 1: A. Stone in the left ureterovesical junction with proximal edema. B. Ureteral urine jet slightly decreased in the left side.
Transvaginal and Introital Ultrasound
We do not typically use the transvaginal and/or introital ultrasound in the standard diagnostic process for urinary infections. That being said, there are cases with diagnostic difficulties where the use of this tool might bring us a lot of information. For instance, female voiding dysfunction, urination urge symptoms, recurrent urinary tract infections and urinary incontinence, may occur secondary to morphological and topographical changes of the urogenital organs.
Introital Ultrasonography
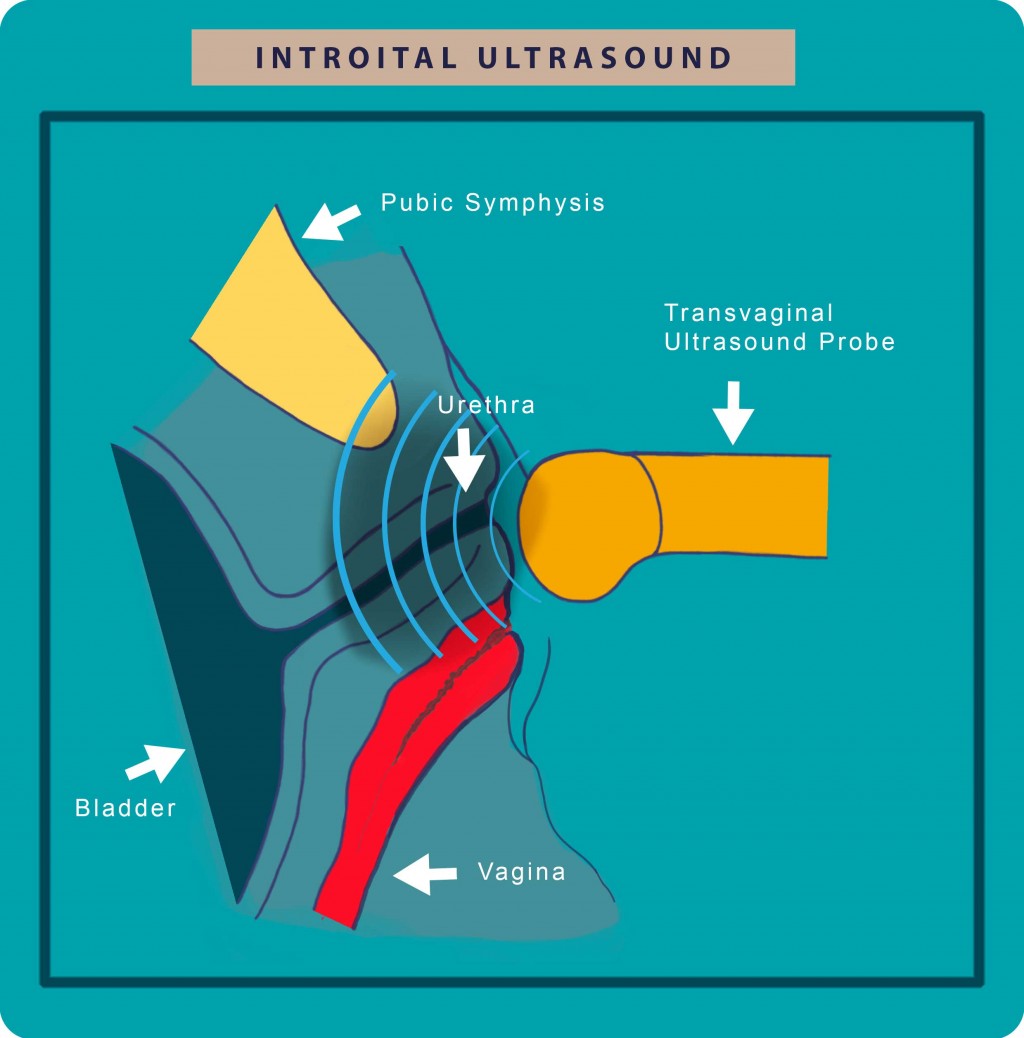
Figure 2: In Introital Ultrasonography, the probe is placed just in front the external urethral orifice with the transducer axis corresponding to the body axis.
We perform the examination having the patient in the semireclining position and the sonograph probe in the same axis to that of the body. Thus, the patient can press adequately which would be difficult if she was in lying or in standing position.
Using the introital ultrasound we may find pathology such as:
- Urethral diverticula
- Periurethral masses
- Funneling of the urethra
- Cystoceles
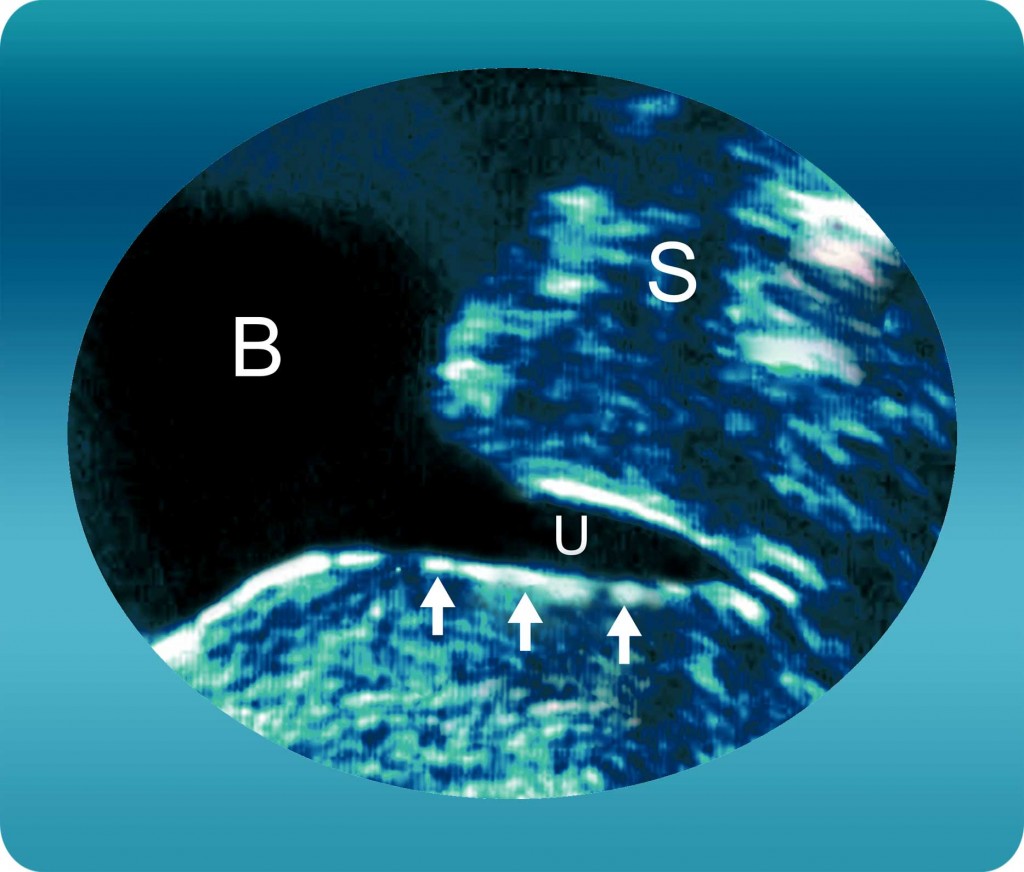
Figure 3: Urethral Funneling (vesiculation) of the proximal urethra during coughing is a typical sign of urinary stress incontinence.
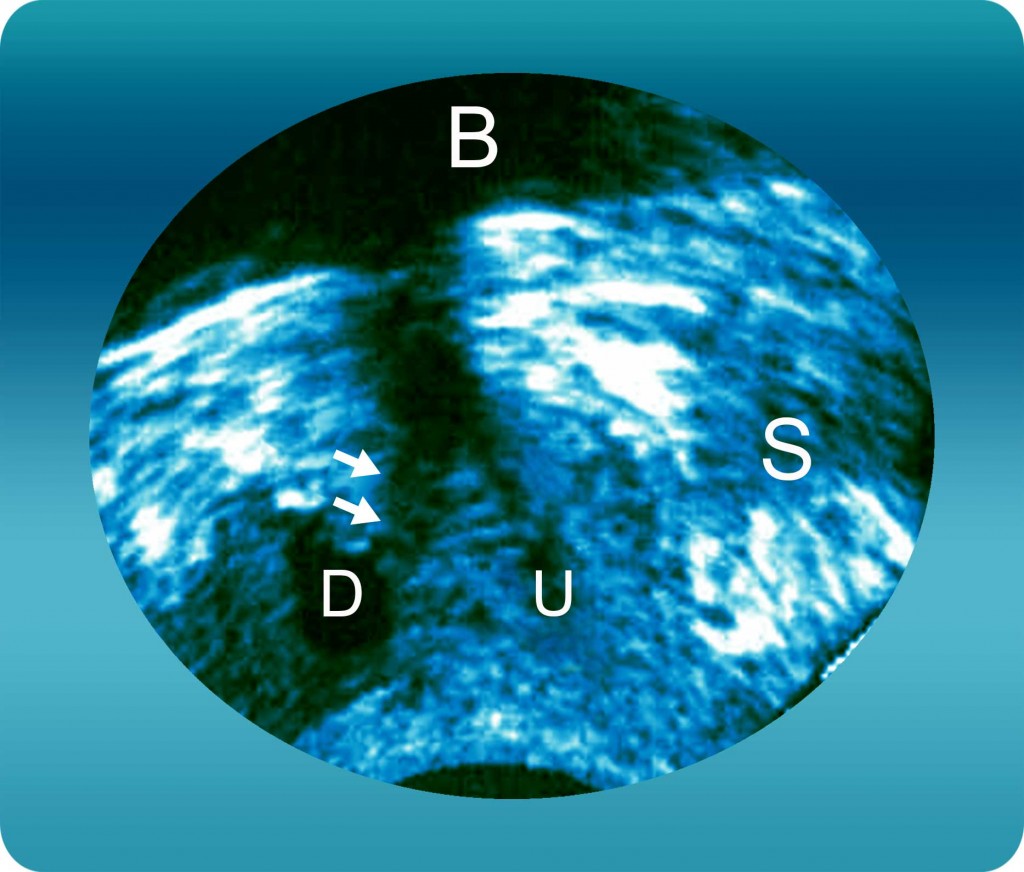
Figure 4: Urethral Diverticula (D) with neck (arrow) arising from the posterior wall of the urethra.
Transvaginal sonography
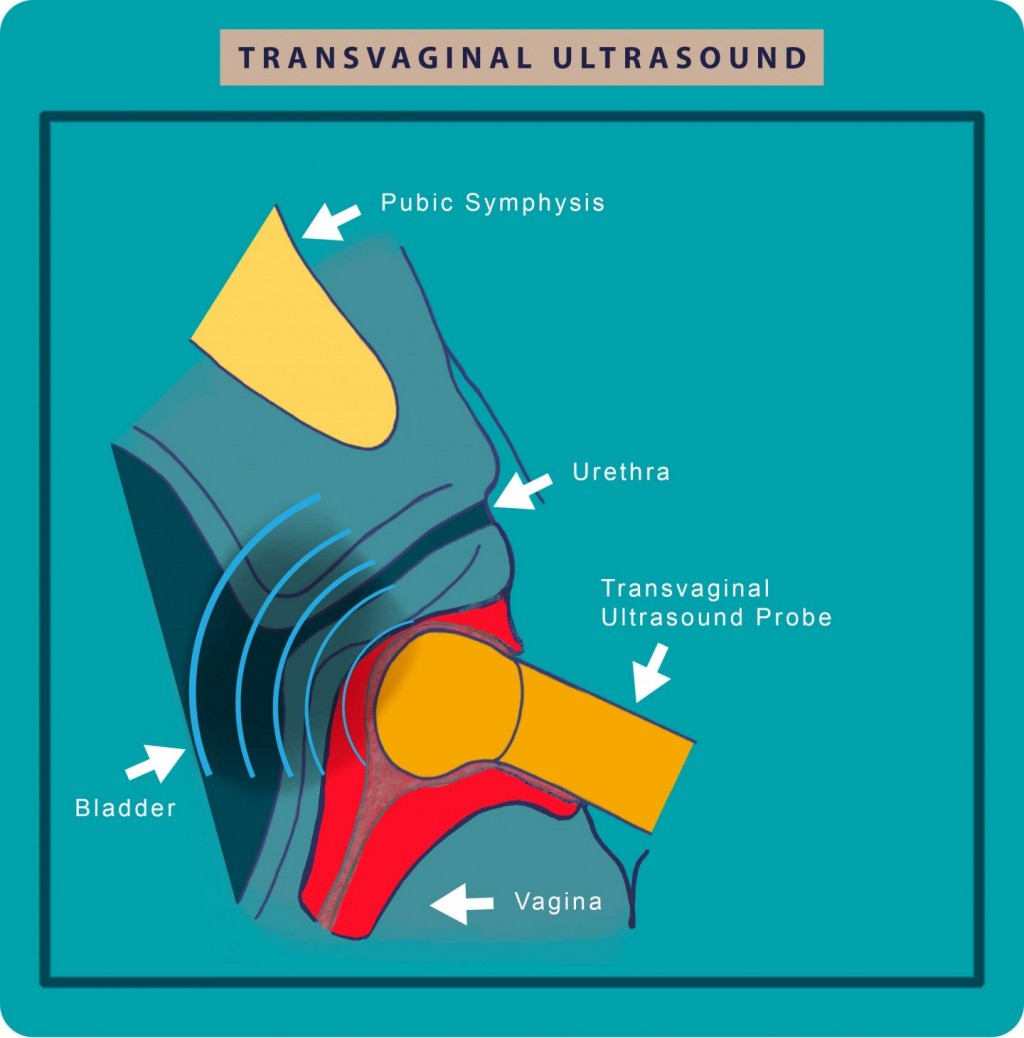
Figure 5: Transvaginal Ultrasound which is especially effective for detecting urogynecological diseases from the bladder and uterus.
The transvaginal ultrasound enables the detection of:
- Pathologies of the urinary bladder
- Abnormal uterus morphology including its appendages
- Degree of urinary stress incontinence
- Morphological and dynamic changes in prolapsed genitourinary
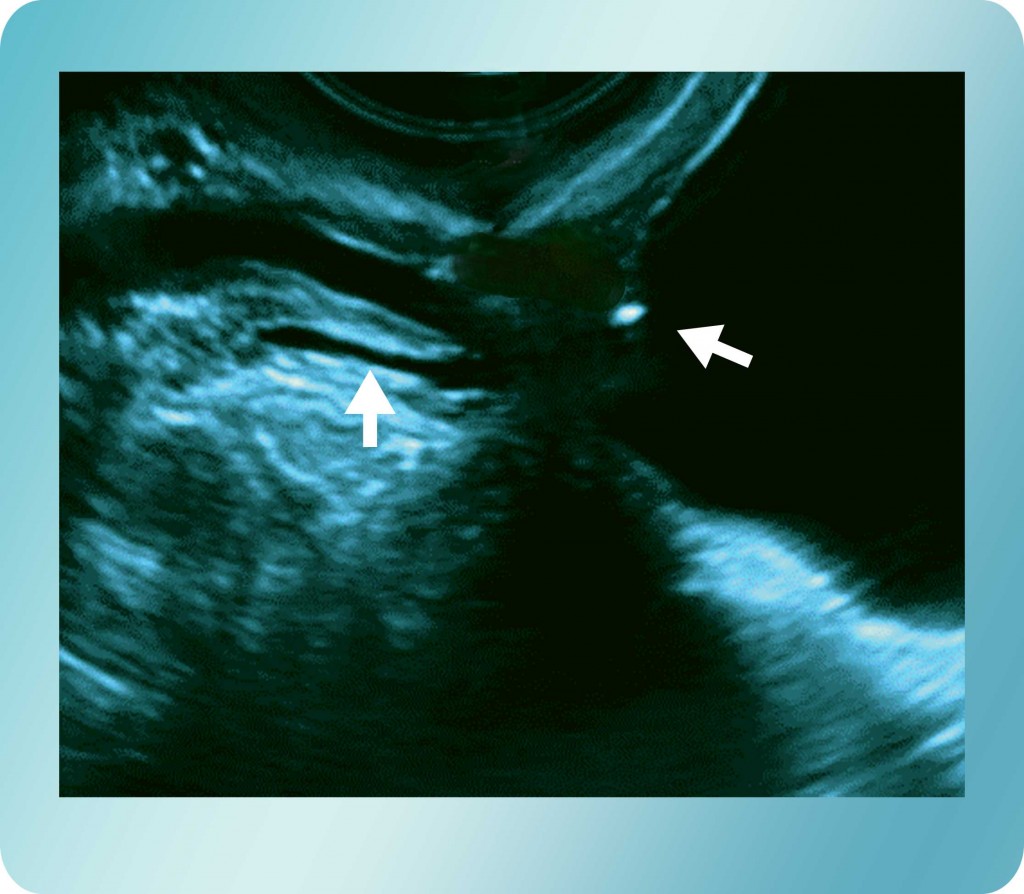
Figure 6: Transvaginal sonogram showing an obstructing stone at the ureterovesical junction with dilatation of the proximal ureter.
C. Radiological Imaging
Intravenous Urography
Intravenous urography is reserved for cases where differential diagnosis is required. It is primarily used when a stone or a mass blocks the final part of the ureter and the other tests give unclear results regarding the aetiology.
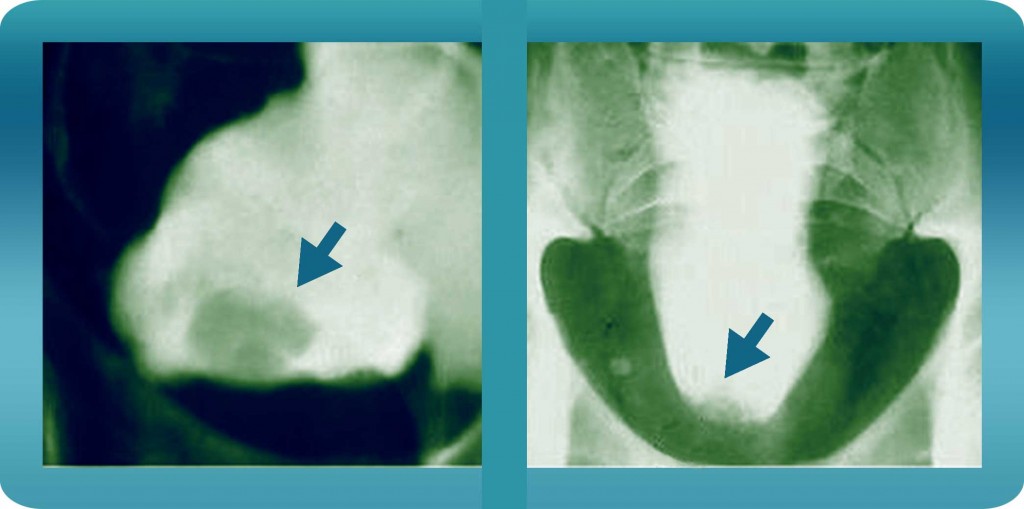
Figures 7 & 8: Intravenous pyelogram with cystography in lateral and upright receptors, showing contrast filling shortage in the base and a deformation of the shape of the bladder, with a “pear” display type, which proved to be glandular cystitis with a concomitant pelvis lipomatosis.
CT scan
For a of cases, the CT scan is considered necessary for differential diagnosis in:
- Intramural bladder pathology
- Problems around the pelvis
D. Flowmetry test
This is a non-invasive test with the use of a device which records the flow of urine while the patient urinates inside it. Under the appropriate patient preparation, it can give us a clear and reliable estimation of the urine flow rate (i.e. how easy or hard the person could pass the urine out).
In several cases it shows problems that might be the cause or a complication of the disease (chronic cystitis). It can offer a useful information about the chronicity of the disease and it certainly is a helpful examination. There are more than a few cases where post-inflammatory urethral strictures maintain and increase the frequency of relapses. There are a number of useful flowmetry results we look for, such as:
- Peak flow < 15 mL/sec
- Residual urine > 50 mL
- Minimum total bladder volume of 150 mL before voiding
These may appear individually or in combination, and they constitute useful evidence when diagnosing voiding difficulties in women.
E. Cystoscopy
Urethrocystoscopy (or cystoscopy of the bladder & urethra) is the main examination for diseases of the urinary bladder. It effectively enables direct visual control of bladder pathology. The modern and technologically advanced cystoscopic devices show detailed and magnified images, allowing the doctor to do things such as:
- Diagnose the type of the disease
- Evaluate the extent of the inflamed area
- Estimate the chronicity of the problem
- Evaluate the type of treatment to apply
- Approximate the length of therapy
Procedure of Cystoscopy
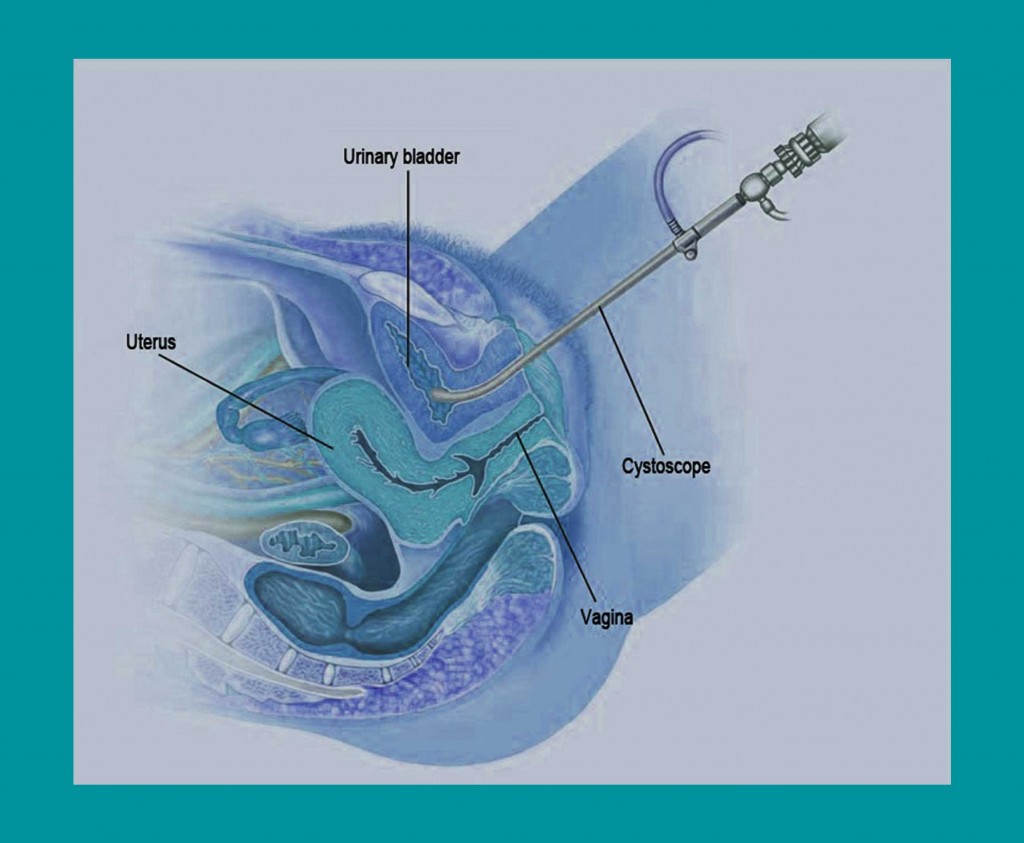
Figure 9. Insertion of the cystoscope into the bladder.
Cystoscopy is a painless examination which we perform in our laboratory setting in the following way:
- We apply a local anesthetic (gel) to the urethra.
- Then we insert the cystoscope, which consists of a thin metal tube, through which the magnifying lens passes.
- This in turn is connected with a special light beam emission, so that the optical image obtained is clear and detailed.
The equipment of the cystoscopies (i.e. the cystoscopes) and the specialised technological light beam sources, create the conditions necessary for proper evaluation.
The experience of the urologist is a prerequisite for the proper evaluation of the inflammation. During the procedure, we act based on the detected suspicious images, and more specifically:
- The lesions may be either limited or cover almost the entire cystic wall.
- In some cases, they require a differential diagnosis, since other malignant lesions may be concealed.
- If during the examination there are diagnostic problems, then tissue sampling from the suspicious areas is used to make the diagnosis.
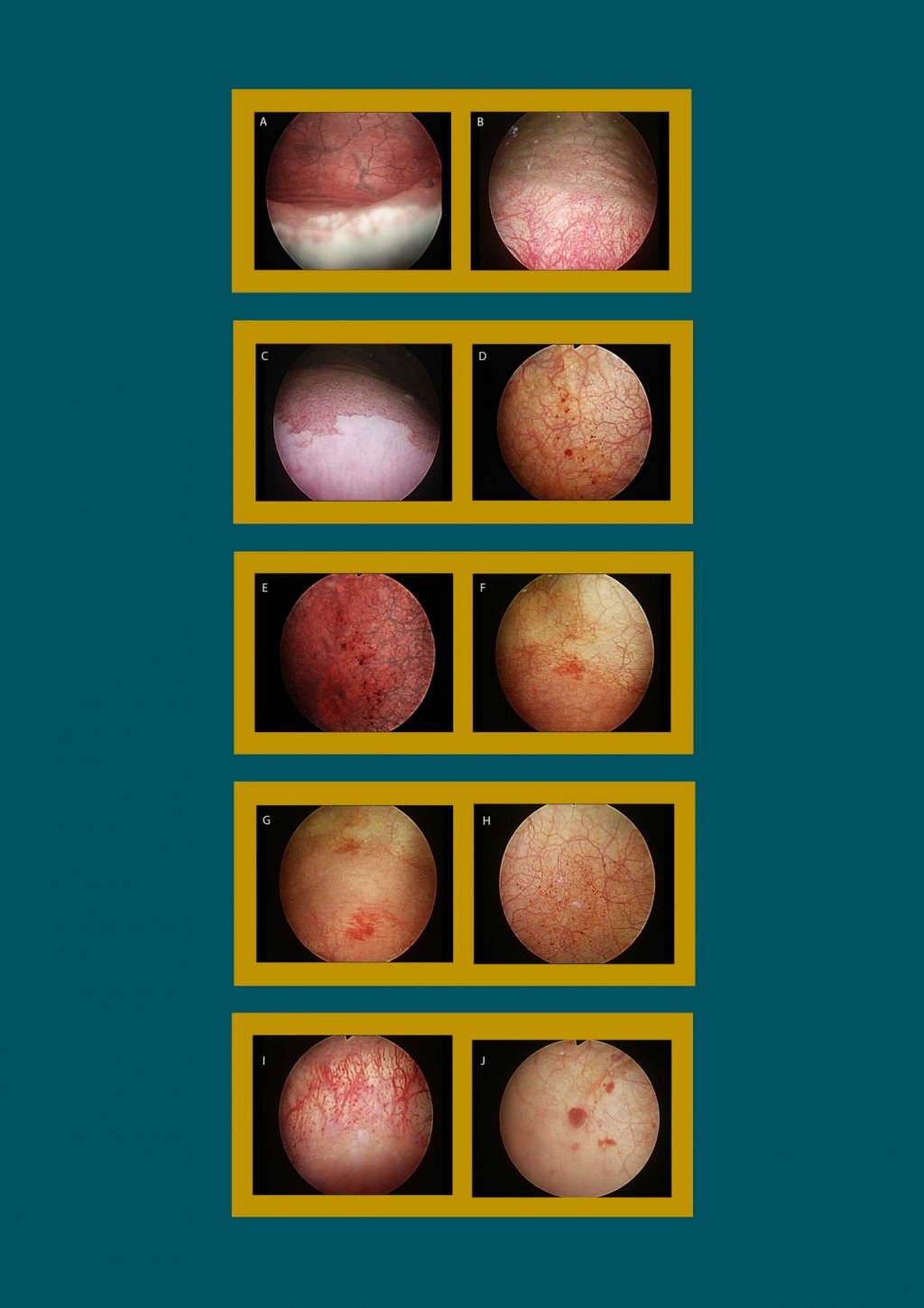
Figure 10: Various forms of chronic cystitis visible through cystoscopy. We can see cases of membranous trigonitis, cystic cystitis, glandular cystitis, erythematous crystalline calcifications.
